This is a continuation of Protein myths so as not to hijack the OP’s thread.
Protein Myths: Continued
Thanks @Ilana_Rose.
@Freefall_Doug - FYI - The reason I follow up like this (the link below) is that I think the “just have more protein” message can be received when - I think - that is dangerous without the “and do strength training” message.
Similar to the “carbs are okay” message. Of course, in the athletic arena, where carbs are used for performance and will be “burned off” immediately - especially for intense (vs. endurance) competition - that message is okay. People that have fat-adapted and can easily switch fuel sources can take advantage of whatever works best for them.
But, without that context, (which “big sugar” does not provide) the “carbs are okay” message can lead to thinking 100 calories of soda is just as good as 100 calories of salmon is a reasonable conclusion.
@RobC I can understand that point of view, and I think that we both agree entirely with the value of resistance training.
On the other end of the spectrum I think too often there is advice given to use protein sparingly when a higher level of consumption may have no negative impact on ketosis for those individuals. We are all our own individual N=1’s, and all of our mileage may vary.
If people are starting from a point of avoiding protein by following macros based on this advice they won’t easily determine what their own ideal level of consumption is within keto WOL.
My ideal combo is both, resistance training, and determining the upper limit of protein consumption that doesn’t impact their level of ketosis.
I think there are two answers here and I think you are dealing with the answer about how to deal with Keto after a few months. (Although I am not sure “upper limit” seeking is better than “definitely sufficient to not be a bottleneck”).
For me, the newbie mindset (and as mine was at the beginning), is still dragged down by past constant messaging that “fat is bad” from birth.
For example - I realized at some point that I was still draining fat after cooking 10 ounces of 80/20 ground beef. Instead, I started adding a couple of ounces of cream cheese to mix with the grass fed fat to make a nice creamy sauce. If I had a “keep protein high” focus - I might have drained the fat to keep different macro ratios and increased my time to fat-adaptation.
During fat-adaptation I think it is important to get that “fat is good” message across and then, once adapted, make sure protein is on point and vary fat to force body fat burning.
I agree some people are pumping iron and doing HP (high protein) e.g. carnivore (0 carb)… which could be different compared to someone who may be e.g. sedentary and diabetic (GLUT4 transporter receptors that recess deep into the cell membrane but also muscle contraction stimulates muscle cells to translocate GLUT4 receptors to their surfaces) so there is a big difference in the methodologies and what the biological processes may be for each circumstance from digestion to protease peptide enzyme breakdown to more skeletal muscle tissue meaning more insulin receptor sites?
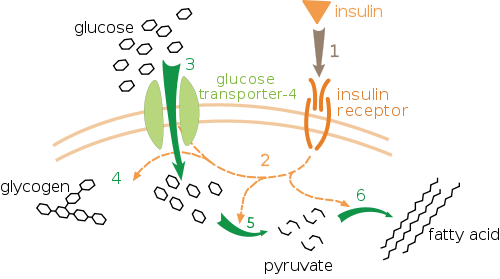
More insulin receptors sites means it’s easier for your body to deal with dietary sugar and perhaps from gluconeogenesis[1] and whether or not it is going to be used directly as fuel, stored as fat and glycogen or pulled from glycogen stores in the muscle tissue itself?
Footnotes:
Abstract: Dietary proteins are believed to participate significantly in maintaining blood glucose levels, but their contribution to endogenous glucose production (EGP) remains unclear. We investigated this question using multiple stable isotopes. After overnight fasting, eight healthy volunteers received an intravenous infusion of [6,6-2H2]-glucose. Two hours later, they ingested four eggs containing 23 g of intrinsically, uniformly, and doubly [15N]-[13C]–labeled proteins. Gas exchanges, expired CO2, blood, and urine were collected over the 8 h following egg ingestion. The cumulative amount of dietary amino acids (AAs) deaminated over this 8-h period was 18.1 ± 3.5%, 17.5% of them being oxidized. The EGP remained stable for 6 h but fell thereafter, concomitantly with blood glucose levels. During the 8 h after egg ingestion, 50.4 ± 7.7 g of glucose was produced, but only 3.9 ± 0.7 g originated from dietary AA. Our results show that the total postprandial contribution of dietary AA to EGP was small in humans habituated to a diet medium-rich in proteins, even after an overnight fast and in the absence of carbohydrates from the meal. These findings question the respective roles of dietary proteins and endogenous sources in generating significant amounts of glucose in order to maintain blood glucose levels in healthy subjects.
Proteins are a source of gluconeogenic substrates and can be used to produce glucose under fasting or a low-carbohydrate intake. High-protein (HP) diets are generally low in carbohydrates and assumed to promote postprandial gluconeogenesis. Previous studies showed that the ingestion of an HP diet led to an increase in the postprandial expression of gluconeogenic enzymes in rats (1–3) as well as fasting fractional gluconeogenesis in humans (4), and amino acid (AA) infusions enhanced endogenous glucose production (EGP) (5). This glucostatic role of dietary proteins has been hypothesized as being involved in their greater satiating power when compared with other macronutrients (6,7).
Under HP feeding, AAs in excess during the postprandial phase are deaminated (8–10) and generate a large quantity of carbon skeletons that are supposed to be oxidized or transformed into glucose. However, the specific postprandial fate of dietary and endogenous AA carbon skeletons has been the subject of very little study. In rats, we recently revealed that only half of postprandially deaminated dietary AAs had been oxidized 4 h after the ingestion of an HP diet (50% of energy as protein) (11), and we assessed that <5% of AA-derived carbon skeletons were used for glucose synthesis. This was achieved by the 15N and 13C labeling of dietary AA and following the tracers in the final products and in glucose. However, we were not able to determine this contribution precisely because we did not measure EGP, and the dietary proteins were traced using extrinsic labeling.
The true contribution of dietary AA to EGP, compared with that of endogenous AA and other gluconeogenic substrates, has not been previously addressed, except by an indirect method in humans (12). The objective of the current study was to precisely measure the contribution of dietary proteins to glucose production in humans by using egg proteins intrinsically labeled with 15N and 13C (13), with the concomitant infusion of deuterated glucose. This original study enabled a precise determination of the contribution of dietary proteins to EGP. …More
This is all a bit deep for me and I am not sure I understand your point (so sorry in advance if I am way off here - not a medical professional so, can be easily fooled).
This seems to be the main positive point (in your reply) of going higher in protein (I think). My contention is that a couch potato might still not benefit from the higher amount of insulin receptors (while taking on the risk of helping growth of things that are not good).
If having more receptor sites is good for weight maintenance, remaining low-weight stable but needing a cane or having to ask for help out of a chair isn’t what I want. Exercising for the muscle and function is what seems important (and will help keep hormones in balance - as far as I know).
Thing about initiating glucagon when eating only protein is glucagon pulls glycogen from glycogen stores in muscle tissue so the liver can convert it back into glucose rather than a diabetic reaching for a tube of glucose or eating sugar when hypoglycemic?
Insulin will not be triggered in such a scenario? (not completely sold on this statement, if so, is the triggering of glucagon first, then insulin better? Further yet, what is going on with the gluconeogenesis [glucose]; is it being stored as glycogen, fat or directly being burned as fuel?)
Another thing I’d like to throw out there is about the backing of high protein.
First, allow me adjust my soap box…
Certain food companies and, of course, protein supplement companies really want positive high-protein studies run, published and well advertised.
They won’t pay for studies and don’t want anything published about the idea that simply exercising on a moderate protein diet might be multiple times better.
Even gyms don’t want these studies. Most of them are working on the basis of way overselling memberships depending on people not showing up. January is the month when most people do (new members and existing members with New Year’s resolutions) and finding a piece of equipment is really difficult - gym owners don’t want that year-round.
So, I don’t have studies that back up adding muscle through exercise before the effects of sarcopenia really take hold is a good thing vs. the solution of raising protein when you notice you are suffering muscle loss. But, my intuition leads me to believe that having more muscle to start is better.
Another thing supporting (I think) that muscle is gained through exercise vs. protein intake…
Think of a 400 pound person that has been on a very low calorie diet (say 800 calories) for 6 months and just came down from 500 pounds.
That means way underfeeding on protein - by far, most calories are from local body fat stores.
BUT - they can still stand up!
Most 200 pound people cannot stand up with an extra 200 pounds on their body.
That 400 pound person has retained a large amount of the muscle they developed carrying around their 500 pound body.
Muscle growth really seems to be related (a lot) to muscles having to adapt to stress (vs. adapting to higher dietary protein intake).
I have a few issues with Bikman’s presentation, especially with how the results he discussed are interpreted.
My first big issue is that I cannot find the human study that he describes near the end anywhere. There is no way to assess his methodology, results, or interpretation. It’s been years now since he made that presentation so it’s hard to fathom why it’s still not in print. Did it fail peer review?
It’s possible that I missed it in my search though I did look quite hard and even asked him for it on twitter. So if anyone else has found the article where he feeds humans protein to assess their insulin to glucagon ratio I’d be very grateful for the link.
Secondly, his big conclusion is that we don’t have to fear too much protein because the insulin to glucagon ratio when people on a low-carb diet consume 1 gram per kilogram of body weight doesn’t change significantly from the normal I/G ratio of that population.
But wait a minute. One gram/kg of body weight IS the standard amount of protein recommended for a ketogenic diet! So, he’s given a population the exact same amount of protein they normally consume in a day and shown that they have a similar insulin/glucagon ratio when given that amount. I’m not really surprised by this result, and I just don’t understand why it’s taken to mean that higher amounts of protein would lead to either the same ratio or the same effect on adipocytes, protein metabolism, or ketone production.
Without his having tested other protein amounts we have no idea at all what insulin/glucagon ratio would be engendered by higher or lower amounts of protein.
I’ll leave this topic of Dr. Bikman’s presentation here for now in the hope that I really have just missed the study and that someone can point me to it so that I can actually assess it. Because without it all we really have is a hypothesis.
@RobC all good stuff, I think this is a great conversation.
I bet there are studies out there, and I wouldn’t refute your position that the primary focus should be an sufficient level of resistance training and exercise.
There may be activity only exercise studies. I found this abstract, but unfortunately the whole study article is pay only. But it does have a good list of citations if you wanted to start searching through them.
Physical activity and exercise as countermeasures to physical frailty and sarcopenia
Let’s say the 500 pound person over-eats protein (excessively) and drops 200 or 300 pounds; then I can imagine all the bariatric surgical grade excessive skin that will accumulate?
”…all of which needs to be catabolized (burned up and not replaced)[1]…”
Footnotes:
[1] How much protein is excessive? How much protein is enough?
Isn’t fasting for autophagy the way around loose skin?
Even so, I agree, at those weights, still would probably need surgery (I think).
I have read about several people at IDM who started out at 400-500 pounds who have not needed skin surgery because they fasted and did weights.
As someone who started in that range I hope it is true. I do fast but I haven’t started weights which I am guessing is essential to do with the fasts as it creates a high need for protein.
We will see in a couple of years. I think it will take that long.
Quoting myself:
Dr. J. Fung:
”…Any protein eaten in excess needs to be converted to glucose or fat for storage. Nine amino acids are called ‘essential’ amino acids because our body cannot synthesize them – histidine, isoleucine, leucine, lysine, methionine, phenylalanin, threonine, tryptophan, and valine. We must get these from our diet or we will get malnourished. There are also essential fatty acids such as the omega 3 and 6. There are no essential carbohydrates. No, we do not ‘need’ to eat 130 grams of glucose daily for our brain. It’s a complete lie. Fasting for 1 day does not cause our brain to become ‘starved of glucose’ as we become blubbering idiots and lose control of bowel and bladder. I would vote that widely circulated ‘fact’ as ‘most idiotic statement’. I have done this 24-hr fast many times, and have not yet found it necessary to clean poo and pee afterwards. …” …More
I do not remember hearing that doing weights was good from the IDM program.
Dr. Fung seems to say fast for weight loss and exercise for muscle gain (and he is pretty black-and-white about it).
So, I do not think weights are essential for the loose skin (and would be counter productive if it drove hunger) nearly as much as focusing on getting autophagy going (no HWC in coffee or bone broth for example - no nutrients during your fasts, just electrolytes).
If you could get some strength training in without driving hunger - the benefit will be (I think) looking more toned at goal. Also, large weight loss will probably be accompanied by large muscle loss (as you lose weight you cause less and less stress adaptations to occur). It is probably (I do not know for sure - depends on age I think) easier to retain some of the muscle you needed to move around at a higher weight than it is to get to goal and try to add it back (seems intuitively obvious but I have not science to back it up).
This statement seems odd to me. When I consume excess protein I get hot and there is also the higher thermic effect of protein. I am not sure if those are actually the same or if getting hot is essentially raised metabolism and the thermic effect of food means that a higher number of calories are being burned while dealing with the protein.
The statement seems to make sense if it was carbs instead.
I am not saying the statement is wrong - just that 100 excess calories of protein will result in less storage (i.e. not produce 100 calories of fat on the body).
While we are discussing this, I think some clearer distinguishments need to made:
-
The sedentary people?
-
The diabetic people? (pre-diabetic insulin resistant and/or leptin resistant)
-
The iron pumping body builder people?
-
The fat adapted ketonaut people?
-
The fasting only sugar burner people?
-
The more physically active person?
And the variant x, y, axis in-between those factors?
That may be in-line with my theory or hypothesis (et al.); your burning it directly (UCP-1) as energy via BAT or brown adipose tissue or the browning (iron) of WAT or white adipose tissue and at the same time burning the VAT or visceral adipose tissue off the internal organs and not storing it as glycogen or fat?
