SHORT VERSION
After embarking on a diligent keto eating style in July 2019, my CAC scores have risen steadily:
55 - Aug 2019
68 - Feb 2020
207 - May 2021
Virtually all of the calcification found (and increases thereof) is evident in the RCA (Right Coronary Artery).
After further research (and considerable angst), I can’t identify any heart-smart course of action besides staying the course and doing exactly what I’ve been doing since mid-2019 when I went keto.
If you’re either interested and/or have any science-based thoughts to share with me (and others in this situation), please enjoy the long version below and feel free to chime in.
LONG VERSION
July 2019: As a 62 yr old male who ate “low-fat” for decades (therefore high carb), I jogged daily, BMI=24, acceptable lipid panel and was generally healthy (i.e., no meds), yet I was feeling “old” … stiff morning joints, nighttime GERD attacks, trigger-finger in both hands, tired easily, soreness after yardwork, etc. I also worried about my wife’s well-being as she was not eating nearly as “healthy” as I was; I thought I could get us both aimed in a different direction.
So after much reading/research (including every episode of 2KDudes), I went full keto in 7/19, tracking every bite for almost a year (Carb Mgr app).
Within weeks I began to feel amazing. Every single “aging ailment” noted above disappeared. And my sense of feeling remarkably healthy again has remained with me for these past two years - now am 64 yrs old and loving life in this restored body.
BTW, I also lost 4" at the waist, 25 lbs on the scale, and my BMI is now 20. HIIT strength training 3x weekly, HIIT-Sprint cardio training. Now weigh 140lbs @ 5’ 9" My strength, concentration, digestion, stamina all now rival my “20 yr old” self. (My wife has followed along, but not as diligently - yet another story.)
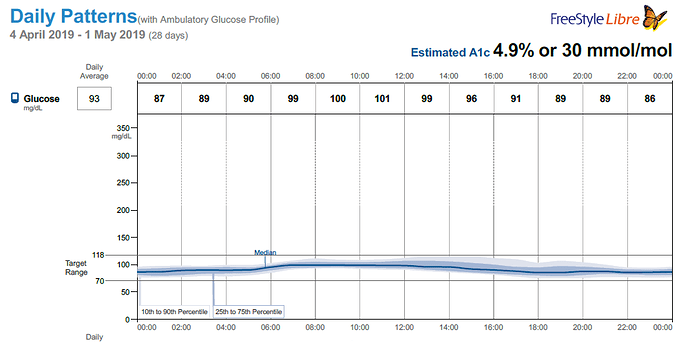
Anyhow, my NMR lipid panel, being a LMHR (Lean Mass Hyper Responder) went bonkers at first, but has since settled down nicely. My most recent results:
TC: 264
LDL: 147
HDL: 108
Trig: 56
Trig/HDL = 0.5
Pattern A particle profile (LDL large/fluffy)
Highly insulin sensitive (LP/IR score <25 - off the chart in a good way)
Since there are a variety of “keto” eating styles, I’ll be more specific. During these past 2 years:
No breakfast other than 1 cup of coffee.
Two meals/day within 6/18 hr feeding window
DAILY MACRO AVERAGES (roughly 1800 kcal) per diligent Carb Mgr tracking:
25g of net carbs *(details below)
93g protein
116g fat **(details below)
Added sugar: 0g
*Note: Net carbs (after fiber) come only from extraneous sources: grilled meats, eggs, bacon, butter, cheese, lots of leafy green garden veggies, home ferments, limited nuts… but ZERO grains, rice, beans, potatoes, breads, corn, etc. and zero “cheating” (not that I’m a fan of that term).
**Note: Fat composition: 37g = 32% saturated; 35g mono, 11g poly, all sourced primarily from animal products; no seed oils; no frying (except eggs in real butter)
DAILY SUPPLEMENTS:
K2/MK4: 500 mcg
K2/MK7: 100 mcg
D3: 125 mcg (5000IU)
Fish oil: 1400 mg (330 mg Omega3)
Magnesium citrate (=500 mg of magnesium) mixed in my daily sea-salted water
 BUT THOSE RISING CAC SCORES FEEL SO SCARY
BUT THOSE RISING CAC SCORES FEEL SO SCARY
Possible next steps:
-
EAT CARBS AGAIN? Makes no sense … cutting out the carbs eliminated the inflammation that I hadn’t even appreciated from all those LFHC decades of eating prior to 2019.
-
CUT BACK ON (SATURATED) FAT? All research I’ve read supports the view that dietary saturated fat is in no way correlated with adverse heart outcomes (or overall morbidity). On the contrary: higher carbs are correlated with bad heart/morbidity outcomes, not fat. Besides: my Trigs are a mere 56 and my HDL is 108 so it seems my dietary fat isn’t turning into serum fat in my blood (i.e., I’m a good example of what the scientific studies have revealed).
-
SUPPLEMENT WITH K2/D3? I’m already on it. Perhaps I should increase my K2 intake further with higher dose (liquid K2 drops)? Well, if the calcium seen on my CAC CT scans represents “scabbing” of the soft plaque into hard protective plaque (with calcium), why would I want to try to leach those stable calcified areas away, perhaps exposing what’s beneath those “scabs” to then freely circulate around my arteries? Toward that end, how much K2 would be too much?
-
TRY TO REDUCE INFLAMMATION FURTHER? Sure, but how does one do that beyond all of the things I’m currently doing? Besides, I have NONE of the symptoms that plagued me before cutting out the extraneous carbs - joints feel great, trigger fingers are cured, focus/concentration is tops, energy level high, hunger level low all day until dinner time. Haven’t even had a common cold in 2 yrs. And even my coronavirus Pfizer shots were non-events (arm didn’t even get sore). By all accounts - confirmed by high insulin sensitivity - I seem to have inflammation response well under control.
To be clear, I’m NOT happy to see my CAC scores rise like this. I was hoping I’d have a 0 score. And when my first result was non-zero, I hoped it would then fall from there. So far, no dice. Bummer. 
But my current assessment is as follows:
Back in 2019, I probably had (decades’ worth) of non-calcified soft plaque in my arteries. Luckily, it never caused an issue (of which I was aware).
And since then, either as sheer coincidence or as a result of keto/K2/D3, my body has begun to “heal itself” by taking on those potentially dangerous soft plaques (which are likely to cause blood clots at some point upon rupture) and holding them in place through calcification, where - once stabilized - they are far less likely to do meaningful harm.
Of course, all of this could be wishful thinking on my part - i.e., assuming away a serious problem of rapidly rising CAC scores!
FWIW, our family internist just moved away so we’re in the process of establishing relationships with a new MD which takes months to get booked. If ultimately told to go on a statin, cut back on saturated fats, take aspirin, or other variations on outdated disproven guidance, I’m not inclined to follow any of those instructions.
MEANWHILE, ANYONE HAVE ANY SCIENCE-BASED SUGGESTIONS/OBSERVATIONS TO SHARE? Would welcome thoughtful fact-based input.
(BTW, in addition to redoubling my research on related topics, I’ve watched a number of Dr Ford Brewer’s posts on rising CAC scores, K2 and such. Interesting perspectives offering some comfort that he’s seen many others go down this same kind of path with rising CAC scores.)

 I can’t imagine having a better Trig/HDL/insulin sensitivity profile, so something must be working well in those veins.
I can’t imagine having a better Trig/HDL/insulin sensitivity profile, so something must be working well in those veins.




 … it’s pretty much what I’m left with for the time being.
… it’s pretty much what I’m left with for the time being.