I’ve been on keto for a good 6 months but don’t lose much weight. I’m insulin sensitive (hba1c of 5.3).i read Marty Kendalls website optimisingnutrition.com (also a low carber) and found out that he prescribes a lower fat, moderate protein and lower carb diet for insulin sensitive people for weight loss. I don’t want to be non keto but I want to lose 20 pounds as well. What do I do?
No weight loss on keto
I would recommend you get an insulin test to see if you have high basal insulin rather than guess at it based on A1C. You may indeed have normal insulin levels and be able to alter your protein/fat ratio. Or you may be producing extra insulin to keep your glucose down. Other than that, give higher protein a try for a while and see if it makes things better or worse.
Is there a specific reason you want to be in ketosis?
Try lowering your fat for a week and see what happens. With this WOE you sometimes have to be your own science experiment.
I agree with Jeremy wholly. Not that I’m a scientist but it makes sense that if ketosis causes you to burn dietary AND body fat, and you already have a lot of body fat, why not lower the dietary so the body can concentrate on burning what it has stored? Again, could be way off base here but it just rings in my head.
Dread1840, that kinda makes sense to me, too. Your body only needs so much fuel. And if you’re in ketosis and burning mostly fat, and at the same time are eating all of the fat that your body needs, there is really no reason for the body to pull from it’s fat stores for fuel.
I’m just a newbie, really, but it seems to make sense to lower the fat intake a little to allow the body to pull from the reserves.
A person would still need adequate protein, not excessive, but adequate, and I would think a good supply of non-starchy veggies would be good as well, for nutrients.
If you are eating low carb (20g or less) and moderate protein, the rest has to be fat. If you lower your fat, you may find yourself pretty hungry. This could back fire in keeping the other 2 macros in line. According to Dr. Jason Fung, the key to freeing stored body fat, is to lower insulin and that is done well through fasting.
That’s true but people who are fat adapted can likely lower their fat intake and be perfectly fine because they are able to burn body fat. My wife and I have both found that too much dietary fat = stalled weight loss. The very metabolically broken may need fasts, but it’s all about what works for you.
I absolutely agree. I am an IM Doc and am helping one of my wife’s co-workers. He weights 458 pounds. To my shock, his labs including AIC were completely normal with AIC 5.2. His fasting insulin, however was 32. The normal range is up to 24 but really it should be 5 or less. He is now fat adapted and is losing weight like crazy. I would strongly recommend getting a fasting insulin, it will be tough to lose weight until that is improved. I never checked insulin levels before and am shocked to see how many people are insulin resistant with normal sugars and AIC.
That works in theory IF your insulin levels are sufficiently low. Otherwise, all you’re doing is denying your body energy it needs because it CANNOT access its own reserves, and the result of that is often a drop in basal metabolic rate (see The Biggest Loser, for example). @richard has posted on this repeatedly, so a search of the forums should find many examples of his sciencing the crap out of this notion that all you need to do to lose weight is reduce plate fat.
If insulin is high, the body will not burn fat, simple as that. So for some folks, who are not able to drive insulin low enough via keto alone, intermittent or extended fasting may help drive insulin down further, and enable them to access body fat.
The important takeaway is that there is NO single right answer that fits every person. Some folks may need to further restrict carbs. Some might need to add fat (and yes, some might need to reduce fat). And some might need more (or less) protein.
So Jeremy is right on target that you DO have to experiment to see what works for you. But there are significant downsides to reducing fat (particularly if you don’t replace it with something else), so unless you’re sure that insulin is low enough to allow access to fat stores, it wouldn’t be the first thing I’d try, personally.
Not sure that being fat adapted equals an ability to burn body fat ‘well’ and keto does not equal weight loss. There are a multitude of other factors ~ the most obvious being insulin sensitivity or lack there of. And of course, fasting will also reduce all the macros!!!
How long do you need to fast prior to getting a fasting insulin test? I’m going in for an annual check up soon and want to get this done. I’ve been doing Keto for 3 months and haven’t lost anything. I know I’m in ketosis. My breathalyzer reads anywhere from .04 to 1.9 BAC depending on the different tweaks to the diet that I’ve tried.
Andrew, this sounds like a catch 22 to me. You need to be fat adapted to be able to fast without hunger, but you need to fast to get your insulin level down and be fat adapted and not hungry! Do you just fast and push through the hunger to get there?
Generally an overnight fast—12 hrs. That is standard for checking cholesterol and fasting sugar levels also. Good luck!
It is really taking in enough calories in fat to provide your body with energy until the insulin level drops. According to Dr. Fung, the fasting insulin should be lower than 13 to fast without feeling bad. It is confusing stuff, you are doing great especially if you are in ketosis.
You would need to check with the lab on that question. Insulin is one of the tests that is in the package of tests I get run periodically, and they usually request that you fast overnight. Again, though, check with the lab to be sure.
As I understand it (as an interested layman, not a doctor or scientist), when you fast, your insulin drops pretty quickly. The first 24-36 hours can suck, likely because that’s the time when insulin is still high enough to prevent access to fat. After that, it gets easier, again likely because your insulin drops low enough to allow access to body fat. So it may be helpful to supplement pure fat (coconut oil, butter, and the like) during the first 24-36 hours to make it a little more tolerable. The goal is to lower insulin, so you don’t want to consume carbs or protein, as both will raise insulin.
Hope that helps!
I have an HbA1c of 5.3 and I am really quite insulin resistant. In fact I have a fasted insulin of 13.8 mIU/l when I take metformin and 19.8 when I don’t. So your level of chronic glucose control, is not a good indicator of how much insulin you need to keep that glucose under control. Some people have an HbA1c of 5.3 and a fasted insulin down around 2 mIU/l so they would be insulin sensitive.
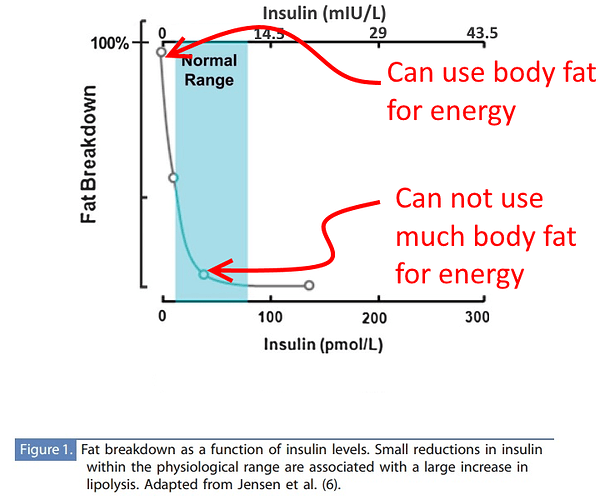
The reason that is a problem is that how much insulin you make when you eat nothing determines how much energy you can extract from body fat.
Along the top you have how much insulin you are making. Let’s say you eat nothing, and your fasted insulin is 2. So you have access to almost 100% of your possible energy from body fat. You can eat nothing and you will burn body fat (if you have enough).
OK Let’s say that when you eat nothing your fasted insulin is 14. Now you have access to only a few percent of your possible body fat release of energy. But you can’t burn nothing you have a brain to keep fed that will need around 600 kCal of energy every day, and you need to spend several hundred kCal just moving sodium out of cells and potassium into them, and breathing and beating your heart, and other stuff. You probably have a minimum requirement of energy around 2000 kCal/day. So where do you get your energy? You burn the only other available energy source - protein.
So clearly how much insulin you make is key to what kind of diet you eat.
Let’s get away from fasting and look at 2 low carb diets. One where you get the minimum protein requirements for body maintenance and glucose production, and then get all your energy from fat - we’ll call that diet “Calories from Fat”. The second diet is one where we restrict dietary fat and increase protein so that we compensate for that extra protein lost for energy - we’ll call that diet “Calories from protein and body fat”.
The first diet we are using protein to build our bodies (and make glucose), and fat to run our bodies - either energy in fat on your plate, or energy you have previously stored in body fat. Your body should tell you when it can’t get enough energy from body fat by making you hungry, and when it has had enough it should tell you it is sated. So the ratio of plate to body fat will be managed by your body which is sampling every possible factor all the time and adjusting your levers. If you are insulin sensitive you won’t need much energy on your plate, if you are insulin resistant you’ll need more. Your weight loss rate will be determined by that insulin status too. And the longer you are at a low insulin level the greater your insulin sensitivity. But it can take up to 10 years.
OK let’s consider the 2nd diet. In this diet we are also using protein to build our bodies (and make glucose), but now we are also getting energy from body fat and dietary protein and the small amount of fat on our plates. Obviously the calculus changes based on how much insulin you make. If you are insulin sensitive then when you reduce your plate fat, your body fat steps in to perform it’s job of supplementing your energy in a famine. If you are insulin resistant and you can’t access much body fat then you will need to eat more protein to prevent your body scavenging lean mass.
3 things happen when you eat more protein.
- You make more insulin - so if you are insulin resistant, you will make more for longer. It will affect access to body fat, it’ll also affect hunger as if draws down glucose, and you eat more protein.
- You make fewer ketones (TLDR;
 Insulin,
Insulin,  Oxaloacetate,
Oxaloacetate,  Acetyl-CoA). Fewer ketones mean you need to make more glucose for your brain - you need more protein.
Acetyl-CoA). Fewer ketones mean you need to make more glucose for your brain - you need more protein. - You make more ammonia. This is quite toxic, so normally we convert it into urea and urinate it out.
Someone who is insulin sensitive can probably thrive on this kind of diet. They dramatically draw down body fat until they have so little their abdominal muscles show up to party.
Someone who is insulin resistant however will end up having to burn more protein to make up their energy shortfall, and that can cause them to need to eat increasing amounts … and then we get to urea synthesis.
Normal humans saturate their ability to make urea at roughly 3.3 g/kg LBM of dietary protein.[Souirce: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC333026/]. In other words above that you slowly build up ammonia until it kills you.
A West Australian trainee paramedic and amateur body builder died a few weeks ago from ammonia toxicity. It turns out that she had a hidden Urea cycle disorder which means her ability to make urea is not as high as most people.
Most people with this disorder are diagnosed as children so her case must have been mild enough to escape detection. She had apparently been on various high protein diets without a problem until she went hard on a protein sparing modified fast to cut for a body building competition and then it was discovered that she had a problem - too late.
7999 people in 8000 don’t have a Urea Cycle disorder, they can likely handle up to 3.3g/kg LBM just fine. But it would still be a good idea on any high protein diet to get a blood test regularly for ammonia in circulation to see if it is building up.
There are experts online recommending 3.5-4.4 g/kg LBM as optimum nutrition … I would say that depends on whether accumulating ammonia is considered an optima.
The TLDR; version is … it depends on your insulin status. Try increasing protein and see if it helps. Might be an idea to ask your physician to add a blood test for serum ammonia every couple of months to make sure you are under your personal threshold for urea synthesis. Certainly if you are above 2.5g/kg LBM I would. But most people appear to tolerate high levels of protein in the range from 1.5-2.5 g/kg LBM.
Available calories per day per pound of body fat?
You’d be wrong. There are a lot of people on high protein diets here. Our Zerocarb crew for example. When I did Atkins Induction in 2004 I went high protein because I was still fat phobic so I ate mostly lean proteins and greens. I ended up giving that away after 2 years because I was feeling nauseous all the time, and craving carbs. I recognize those now as respectively … ammonia accumulation, and reactive hypoglycemia.