Peter Attia has a podcast called “The Drive”. I’ve followed Attia for years and respect his opinions. I’ve also been following Dave Feldman for a while and he has a novel idea about the lipid system. Peter Attia interviewed/debated Dave Feldman. Most of Attia’s Podcasts are about 1hr. This one is 3hrs. I’m most of the way through it and my head is going to explode. I’ll need to read the show notes and relisten once or twice. I’d love people’s thoughtful discussion here. But this is deep dive stuff so it could be difficult to discuss here. @richard have you had time to listen? Thoughts?
Attia Feldman podcast
I read some of the show notes. I stopped following Attia way back when I realized he had tons of cognitive dissonance going on, he BELIEVES in the LDL/LDL-p theory and nothing will change his mind (eg, he takes a low dose statin because he thinks it’s “healthy”), and he’s a (in my opinion) supercharged, overbearing Type AAAA personality.
I’m not sure I can listen to 3 hours of that. I may give it a shot, though, once I get finished listening to my latest book.
Here’s a transcript:
https://peterattiamd.com/davefeldmantranscript/
You can find more on Dave’s site:
I think Dave’s personal experimentation is fascinating and hope he continues to collect more data on himself and others. I’m inclined though to give more weight to Peter’s interpretation of the mechanisms in play due to his educational background, clinical experience, social network/mentors and paid staff supporting his efforts to monitor and interpret research. I also respect Peter’s care to explain his reasoning and the degree of uncertainty in his beliefs.
In this case Peter’s views on LDL cause me concern as mine was modestly high pre-keto and it has gone up significantly though not really hyper responder level. Not enough to make me reconsider statins but enough that I will continue monitoring my LDL (particle sizes/counts too) and other risk factors such as inflammation while testing approaches like tweaking my sources of fats.
I don’t know what my LDL-p numbers are. But after listening to both of them not knowing what they are is cause for concern. If normal->yay. If high->???
I’m only about half way through the episode. One thing that stood out to me is what should a LMHR do if they were seeing high A1C before LCHF and are now seeing their LDL and LDL-p skyrocketing. They certainly don’t go back to SAD. Do they back off on the saturated fat–switch to a leaner version of low carb? Should they go on an LDL lower drug? I refuse to believe that our body can’t function normally without help from pharma.
The other thing that struck me is that Peter really came across as a jerk at times in this episode. I’ve followed him for many years and this is the first time I’ve really seen this in him. He’s a smart dude and he knows a heck of a lot about this, but there’s no need to be a jerk about it. Reminded me of the arrogance that got us into low fat. Hats off to Dave for not losing it. I’m going to listen a few more times just to make sure I’m not misreading the tone. I feel like a kid that just found out Santa isn’t real.
It felt a bit like that for me too. Right from the get go in his introduction where he was explaining in advance when he thinks Feldman is wrong in some areas.
I haven’t listened to the whole thing yet… TBH, I liked reading Attia’s old website/blog more than listening to his podcasts. He could edit the tone of those better than with a podcast…And it was waaaay less time consuming.
I haven’t completely listened to it but did read the show notes a few times (because it is faster). I typically respect Peter and what he offers. But I have never like his take on cholesterol. I am really fascinated by Dave and think he is so brilliant. So when I started listening to the podcast, I was getting upset by Peter. I wonder if its because he is causing me to challenge my beliefs and I am resisting it? Either way - I had to stop listening to it as I was getting annoyed.
I am actually starting to get fed up in general by the experts in nutrition lately. I was really disappointed in Dr Rhonda Patrick’s podcast on Joe Rogan (who I really look up to). I was looking forward to hearing her debate on the carnivore diet and why it was bad and felt she offered nothing other than “its untested”…I remember her skepticism way back in the day on keto diet being a complete diet as well. She talked and talked about carnivore being nutritiously incomplete but then in her own diet - she supplements a lot! How is her diet any more complete if she’s always supplementing it? She kept saying just to do fasting…but you can only fast for so long! How are these people supposed to re-feed if every time they eat a vegetable, it causes stomach upset? Why is so hard to believe that this might be necessary for some people, just like being a pure vegetarian might be beneficial for people in recovering their health?
For the first time in years, I have actually lost faith in a lot of people I used to respect just because they all seemed so close minded. I may need to take a break because all they have done is made things a hundred times more confusing especially when all of them after they passionate debates state…I don’t know.
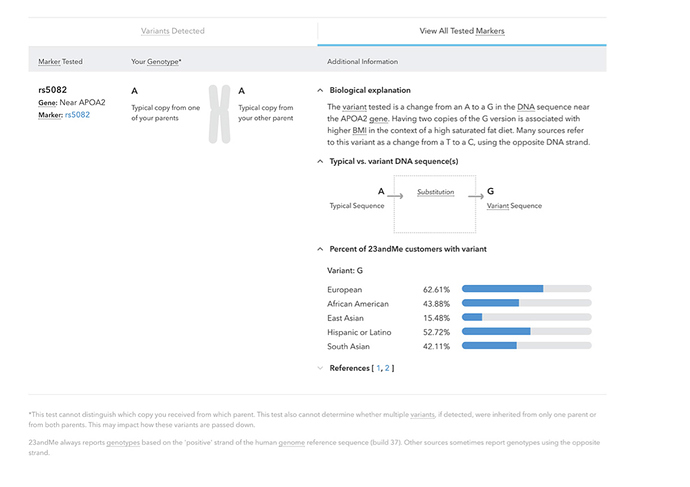
I agree! Back off the sugar and processed carbohydrates? The polyunsaturated fats and saturated fats ratios are seemingly individualized based on genetic herediary attributes of geo-demographic ancestral heritage. Those ancestors living more towards the equator will be eating more plants, those inhabiting less dense vegetation will be eating more meat than plants! This may explain why the ketogenic diet does not work for some people (unless the correct adjustments are made?) while a vegetarian diet works better for others? Blood sugars out of wack? Can’t lose weight? Blood work looks out of whack? May start looking at genetic testing? or could it be a matter of gut flora microbiome ratios or something like e.g. leaky gut?
”… Conventionally, LDL-C is estimated by the Friedewald equation, obviating need for an ultracentrifuge. This equation is based on an analysis of 448 patients from 1972 and estimates LDL-C as (total cholesterol) – (high-density lipoprotein cholesterol [HDL-C]) – (triglycerides/5) in mg/dL. …” …More
Related:
- Apolipoprotein E – ApoE explained: We all carry two copies of the APOE gene. The combination of alleles determines our ApoE3 genotype.
There are six possible combinations (genotypes) for ApoE:
- E2/E2
- E3/E3
- E4/E4
- E2/E3
- E2/E4
- E3/E4
Panic has set in. Need advice!
My bio numbers went wacky disappointed
18 months keto and A1c is going up!? Need encouragement
Thank you so much for posting this! Several times over the last year I’ve thought that it would be interesting to hear a conversation between the two of them.
Will look this up.
The show notes present 3 reasons why Dr. Attia thinks Feldman is full of crap.
Feldman makes clear, at the start of the podcast that he is not a lipid expert. He has a theory, he is an engineer, not a doctor or a biochemist, yada yada. Attia’s three reasons are, if we’re being somewhat Feldman biased, a bit nitpicky, and might be better answered by someone like Dr. Bret Scher or maybe some enterprising biochemical researcher who subscribes to the Feldman theory.
If I am honest, I find Feldman’s theory plausible, because the energy transport theory gives all these lipids a reason for existing, other than making us die from CVD.
If you look at old Attia posts, you’ll find he tells people with high LDL-p to add back in monounsaturated fats and stay away from saturated fats. That’s another reason I stopped following him, as there are NO studies indicating this is true, especially for people who are eating low carb.
The main issue I have with Attia is that he is the consummate physician, which means he has a God complex: I KNOW I’m right. Whereas Dave and others, such as Ivor Cummins and even the 2 keto dudes are basically engineers. They KNOW they are wrong and are fumbling through the data. Attia starts with LDL (or LDL-p) = bad, whereas an engineer says, what does the data say and are there alternative explanations?
A case in point is just reading some of the transcripts: Attia talks and talks and talks, Dave gets a sentence in, Attia talks and talks… And Attia does stuff like summarily dismiss the CAC score, implying it is useless.
This apparent omnipotence has come through in his writings, for a long, long time. That turned me off and still does.
I like people who admit they might not be correct. Attia doesn’t. Dave and Ivor do. (As does Malcolm Kendrick, who I think may have the best explanation of what really causes heart disease.)
Anyway, that’s my diatribe for this. I’ll download this if I can to my podcast app and see if I can listen to it. It will take a while, though.
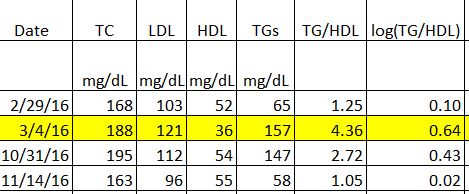
I find his theory plausible also. If you look at the first two lines below, the uppermost was taken after 12 hours fasting, the next lower line (in yellow) was taken the same week after 4.5 days of fasting. I did this before Dave came on the scene, but Dave’s theory explains why this happened. (Note that I think LDL-p went up during this process, but only have that data for one of these.) The whole “LDL = bad” theory does not explain this, nor does it explain the many studies where LDL does not correlate well with heart disease.
These are my exact thoughts. I can’t believe that the normal expression of ldl-p lipids is bad. The anecdotal evidence that they transport fats based on Feldmans self experimentation seems to support this. The lean mass hyper responders are an interesting population. Attia thinks they are at risk for CVD. I would think that it would be a simple thing to look at CAC scores for the ones that have had elevated LDL-p for some time and draw inferences from that. Anyhow I’ve listened to almost the entire podcast once w/o notes. I’ll need to listen again with notes. I truly respect both their opinions and think they are both searching for truths based on their education and life experiences, of course bringing with them some biases. I hope this is the first of many contacts/podcasts between them.
One other nonconsequential thing that bothered me was Attia disliked that people went after Keys as being a bad guy when it was just bad science and he had good intentions. The same can be said of many people in the history of the world that cause heart ache.
We will likely never know who is right for many years, if ever. One thing Dave has done, though, is make it clear that the “cholesterol”/lipid system is very dynamic. When they do studies on lipids, they assume that the person has had that level of lipids for months, years, decades. As shown by the above table, mine change change radically in days or weeks. Dave goes much further than this, showing astounding changes in very short time periods. For this reason alone, even if he’s wrong, he’s done the world a service.
I agree whole heartedly! The medical profession prescribed medications (statins et. al.) based on very dynamic numbers that could have been affect by a number of things from illness to short term diet among many other things.
“I had good intentions” is probably second to “I vas only following orders” as an excused used for great harm on society.
Feldman’s observations on coffee make me wonder how many folks on statins would not have been prescribed them had they taken a couple weeks off from caffeination prior to their last high stakes lipid panel.
It looks to me like Dave’s position is there is a lot of evidence that LDL cholesterol is not the primary cause of CVD. He has found that he can readily manipulate his LDL measurements over periods of a few days which further calls into question using LDL measurements as a measure of disease risk.
I think Peter’s position is CVD is a complicated process and while LDL alone isn’t causative it is a major risk factor. I suggest road accidents as an analogy. Driving fast or drunk doesn’t cause accidents but they are major risk factors. One can do both and not have an accident. But add in an unexpected event out of our control, say a deer jumping into the road, and these risk factors can instantly become very relevant.
In the case of CVD it is increasingly acknowledged that inflammation is a major contributing factor as it affects the rate that arteries develop cholesterol rich lesions. If on a keto diet ones LDL goes up, heart disease risk could be decreasing if inflammation goes down sufficiently. But imagine a hyper responder with super high LDL gets an infection or some other unpredictable factor causes a major inflammatory response. If so, the high LDL may now be contributing to the disease process. Moderate LDL isn’t mandatory but it is still desirable.
In general keto diets improve most risk factors for CVD such as hypertension, obesity, inflammation, hyperinsulinemia, etc. LDL is a factor that can move in the wrong way even when everything else is getting better. Balancing the tradeoffs needs to be done on a case by case basis and our current state of knowlede/science is insufficient to do this well. And most people, including physicians, have a very incomplete understanding of our incomplete science which contributes to poor decisions and poor outcomes.
I think an implicit assumption in Feldman’s observations, as well as those of other LC advocates who are skeptical of LDL, is that insulin resistance matters more than the LDL numbers.
Consider, that half of the folks who have heart attacks, do not have elevated LDL. The High HDL-Low Tri pattern signals low insulin resistance. The Feldman Challenge that goes out on the Twitter and has yet to be cashed is to provide a non-drug, non-gene study that controls for high HDL, low Tri, and still implicates high LDL.
The short of it is, ketonians have not been studied much for CVD.
My position on statin use for High LDL with high HDL and low Triglycerides is that someone would have to show me the science demonstrating an all cause mortality benefit to statin therapy, not a CVD mortality benefit. All cause, because dead is dead, while CVD is survivable. To date, to my knowledge, the only improvement to ACM from statin use is to men under 50 (check), who have already suffered a heart attack (whoops). As I do not fit that demographic, I will not take statins.
My endocrinologist was very concerned about me having FH. Fine, even if I have the genes for it, let’s look at other risk factors. My dad never really moved beyond pre-diabetes, is 74, has never had any CV event, but is suffering from Alzheimers, despite cholesterol levels that have been elevated for his entire adult life. My dad was put on a statin recently, and NOW, at 74, has been prescribed metformin, as a precaution. Hmmm… It’s known that statins increase your likelihood of developing T2DM. Part of why I don’t want that.
My uncle did have a heart attack or two some time in his late 40s or early 50s. He smoked, had real T2DM, and died of lung cancer before he turned 70.
My dad is a first level relative. My uncle is a second. My uncle engaged in multiple risk factors, my dad fewer (he smoked into his 30s), and me currently, fewer still (no smoking since a couple in high school). So, should I be worried about the FH? If so, should I worry about the LDL or just avoid things that produce chronic inflammation, and will make the LDL more dangerous? I think I’m gonna opt for not worrying about LDL-C, LDL-P, ApoB, Lp(a), or anything but inflammatory markers and insulin resistant measures.