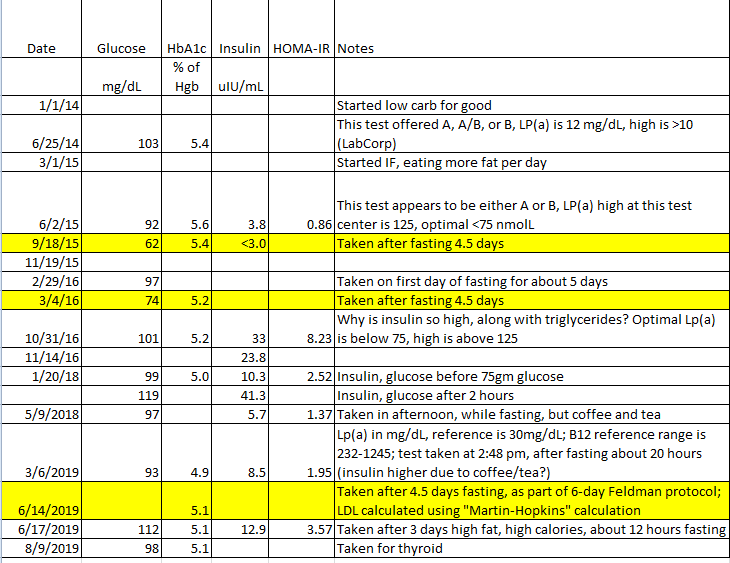
Just back from getting the latest set of monitoring blood tests. There is good stuff and areas to work on. The HOMA-IR calculation does not look good. Time to re-assess the foods moving forward.
Persistent insulin resistance can be the underlying reason for a prolonged weight loss plateau.
Calculating insulin resistance using the HOMA-IR calculation.
Materials for HOMA-IR:
- Fasting Insulin blood test result (mU/L)
- Fasting Blood Glucose taken at the same time (mg/dl)
Use an online calculator: https://www.thebloodcode.com/homa-ir-calculator/
e.g. 12 (insulin) x 94 (blood glucose) = 2.8
Interpretation:
Less than 1 = not insulin resistant/ insulin sensitive
Greater than 1 = possibly insulin resistant
2 = insulin resistant
Greater than 2.9 = significant insulin resistance
Inflammatory hysteresis
hysteresis: the phenomenon in which the value of a physical property lags behind changes in the effect causing it,
The longer [a person] remain on this or any other “high inflammation” diet, the greater the cumulative oxidative stress, and hence also the greater the permanent damage incurred to the organism becomes.
Fig1. The longer you spend on a “high inflammation” diet, the more long-term “damage” you do
Long term on a high inflammatory diet takes time to reverse. It may not be fully reversible. Then it becomes a management proposition that includes not returning to a higher inflammatory diet.
Forum link for people who have been stuck, wondering around, on a plateau: https://lihfliving.com/community/ih/
The editor of the linked forum is particularly interested in the stories of peri-menopausal women who have stubborn, non-shifting body weight concerns.
e.g. plateaus reported in here: The Science Behind Dairy Preventing Weight Loss
A key step to consider trying to achieve weight loss goals is to experiment with removal one of the keto diet’s staple foods: dairy. Lots of discussion in this/our forum (below).
https://www.ketogenicforums.com/search?q=dairy%20weight%20loss%20stall