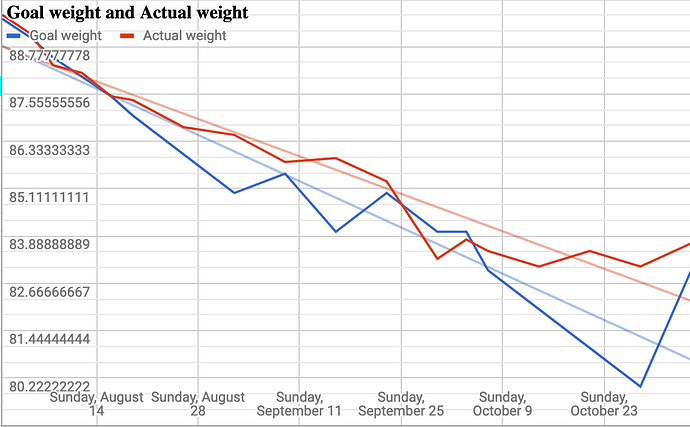
Things started well in 2016 when, in my first 10 weeks, I exercised a lot, ate relatively low carb (but still, heretically, ate some fruit) and lost 10kg. I maintained below about 82kg for nearly a year. This chart illustrates some portion of that lovely decline back in 2016:
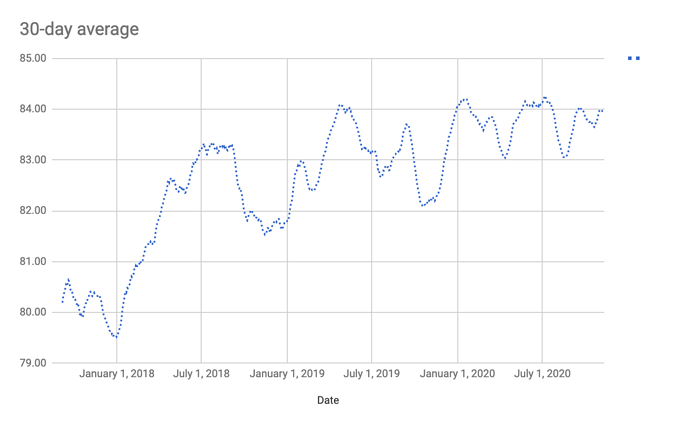
A couple of years ago, I noted substantial weight gain that may or may not have been precipitated by a few days of steroids for sudden hearing loss (I’m ok now, it resolved itself and the steroids weren’t necessary to fix it.) That was sometime in December of 2017, and as you can see in my rolling 30-day average weight chart below – which I measure nearly every morning – there was a weight gain since then which never reversed itself.
I’m not happy with the trajectory; I’m now averaging 84+ kg, and my starting weight before all of this was 93.5kg. So despite avoiding carbs, and with little in my dietary habits fundamentally changing, I’m at a weight that’s now uncomfortable for me.
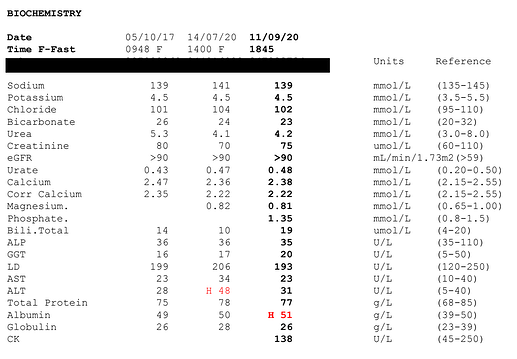
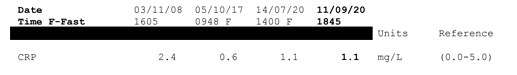
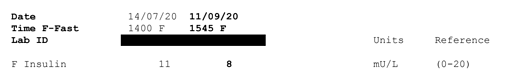
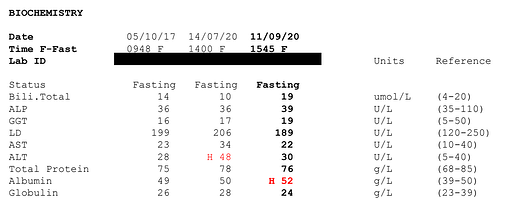
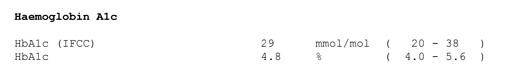
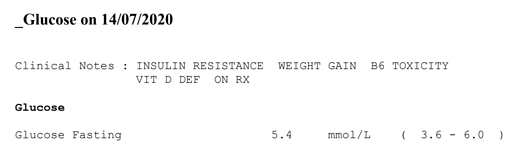
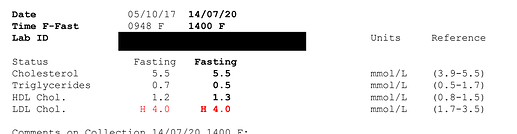
My bloods are all good, except, weirdly, the latest glucose result which is 5.4 here in Australia. I never had anything higher than 90 while living in the US. Could be an anomaly. I checked loads of bloods back in the US, including ApoE and advanced lipid profiles amongst many others. Happy to include them if anyone would like:
Anyway, I’m at a bit of a loss as to what I can do. I’ve tried intermittent fasting, single set to failure training, loads of cardio, no cardio, and various levels of stringencies on low carb. I’ve cut out alcohol except for 1 night per week (which for the eagle-eyed among you explains the improvement in ALT between July and September) and in the past I had extended periods with only black coffee, fearing that half and half milk or even cream was preventing my body from losing fat.
The bottom line is, I suspect I’ve heard every suggestion given to every newbie and every veteran, and I’ve tried probably all of them. One thing that has changed but doesn’t really explain the results is that I’ve been somewhat more sedentary this year as a covid refugee in Australia; back in NYC I walked a lot more. But it’s not correlative.
My diet recently has been 2 high fat cappuccinos (usually made with cream) by mid-afternoon. Then perhaps 3 eggs and some cheese. Very occasionally this might include hollandaise and salmon and avocado. The big meal is usually animal protein with a vegetable like cauliflower+broccoli rice, eggplant, broccolini, or similar. Dessert might be an allulose almond flour slice of cake, or some “well naturally” chocolate sweetened with stevia/erythritol. Or no dessert at all.
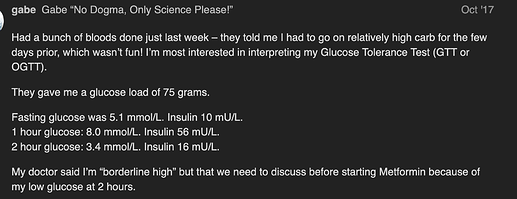
I wonder if anyone has successfully dealt with a similar long-term stall/gain. Is this just my Phinney weight? I’ve had my T checked and in the past Free T was low, but now all seems normal. My vitamin D is great. Perhaps this is where my body wants to be, given my level of insulin resistance? And I’m definitely insulin resistant, an OGTT in 2017 showed as much.
I should note that my doctor is low carb friendly, and he basically shrugged. He’s not worried about my numbers nor my weight. My rheumatologist, on the other hand, would like me to lose weight to take the strain off my poor knees. He might send me to an endocrinologist but I’ve seen one before and I don’t think there’s much they can do.
Would appreciate all constructive criticism. I’ve gone pretty deep with bloodwork and research in the past, and happy to consider anything I may not have thought of.
Tagging @richard because I wonder if you have seen similar cases in your extensive keto journey?