@gabe Thank you for your fulsome reply. You’ve raised several points to unpack…
1 - Whether one’s doctor is a helpful source of medical insight and guidance varies widely. Perhaps yours is not. But just because your physician is stumped - and is willing to leaves things like that - doesn’t mean the test itself is irrelevant.
2 - Then again, if indeed it is a worthless exercise, I’d suggest you cancel your next one slated for this week and refuse any in the future. Why waste your time, treasure, and blood?
3 - My understanding is that high LDL-P counts (in isolation) are not especially meaningful. But since your LDL particle size is concentrated in the small/dense variety - following Pattern B - then, yes, I understand this is fairly important to know. The current position among lipidologists who closely research such things is that, no, this is not a good lipid profile for heart health. So, back to your point, then what?
4 - Okay, here’s what: An individual with Pattern B (small/dense LDL particles) would be wise to pay special attention to their eating and exercise habits … and Gabe, it sounds like this is precisely what you are doing. That’s excellent. You’re a wise man.
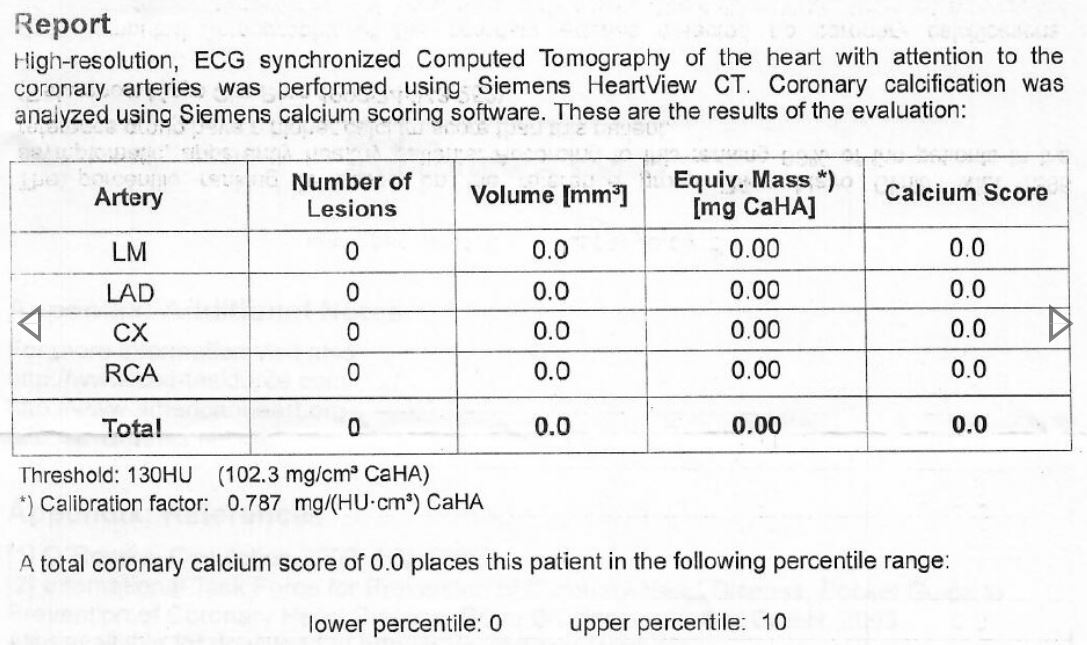
5 - Happily, based on your CAC results, you apparently have no discernible calcium damage appearing in the arteries that support your heart. Double excellent. As @ctviggen rightly notes, the CAC is the only test that shows you actual heart disease progression caught in the act. But I disagree with his conclusion that, therefore, the other sources of information about what’s going on inside your veins is irrelevant in monitoring heart health. (Besides, you can’t safely get a CAC x-ray every other month if you were so inclined, so many other biomarkers are useful as practical tools to keep abreast of what’s going on - especially as you make significant changes in lifestyle.)
6 - Regardless, I’d guess that your NMR results - as disappointing as they must be for you - do in fact provide an invaluable “shot across the bow” in the sense that they suggest your body is more prone to heart trouble than the average guy. If it were me, I’d be motivated to take especially good care of myself. Perhaps others have more tolerance to eat like crap than you do. And, for your 3 years of low-carb eating, it’s likely you’ve dodged some of the damage that would have otherwise been accumulating over time. Triple excellent!
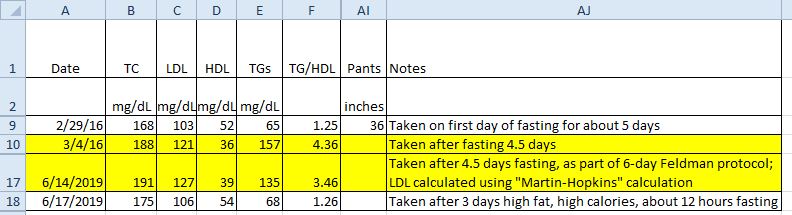
7 - Whether going on/off saturated vs monosat fats (or whatever other n=1 trials you care to try) might be helpful or not is a personal choice. But if I were in your situation, I would test regularly before/during/after such self-experiments (as it sounds you’re inclined to do) to see what I might learn about how my body reacts. Yeah, the tests might provide additional relevant information along the way.
Gabe, if your reaction to the NMR as being a waste of time is rooted in your disappointment over what the results are telling you, I certainly understand and empathize. After 3 years on keto, I’d certainly feel the same way with similar lab reports. But knowing what you know seems extremely worthwhile.
On the other hand, if you truly feel it’s irrelevant, this would be a good time to stop wasting your time and money on getting yet another one to toss into the file drawer.
Regardless, I do wish you the very best.