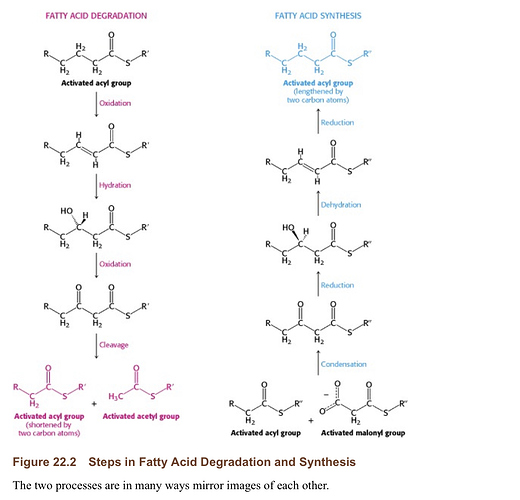
Saturated fats are more readily oxidized by the body of the dietary sort (per Dr. Phinney) than polyunsaturated fats which are more prone to be stored. Immediate oxidation of saturated fatty acids (similar to medium chain triglycerides) just ingested rather than stored (fatty acid turn over pool) then oxidized.
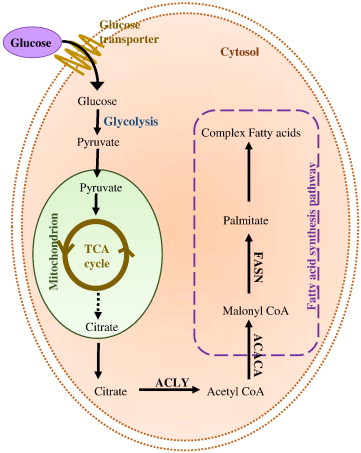
Quid Pro Quo (Adipose Storage of Fats: Carbohydrates vs. Dietary Fat): DNL (De Novo Lipogenesis):
Same with carbohydrates they are not going to be stored (immediately oxidized); as fat in adipose cell tissue if kept under a certain threshold when ketogenically fat adapted, so if you carb up a little, it is more than likely going to be burned (oxidized) for energy (TEE) rather than stored or less likely to be stored (immediately oxidized) in adipose tissue as it would be on a SAD diet. And according to the science on DNL, it is not possible unless your eating an enormous amount of carbohydrates over a long period of time? In other words trying to defeat being in ketosis is not as easy as you would think, once fat adapted (27 weeks/6 months)? There is much more to this than simply depleting glycogen stores and making ketones?
What I’m trying say here is you don’t magically pop out of being fat adapted if you occasionally eat big sugary carbohydrate filled meal! Just stay away from high fructose corn syrup or HFCS?
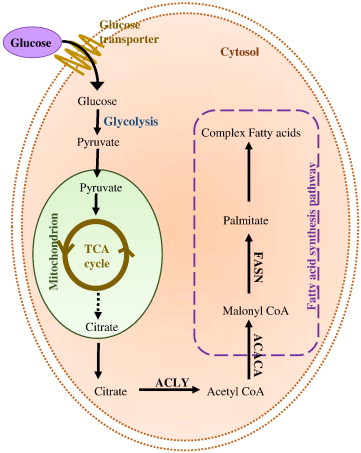
image link
image link
References:
[1] De novo lipogenesis in humans: metabolic and regulatory aspects: “…The enzymatic pathway for converting dietary carbohydrate (CHO) into fat, or de novo lipogenesis (DNL), is present in humans, whereas the capacity to convert fats into CHO (carbohydrates) does not exist. Here, the quantitative importance of DNL in humans is reviewed, focusing on the response to increased intake of dietary CHO (carbohydrates). Eucaloric replacement of dietary fat by CHO (carbohydrates) does not induce hepatic DNL to any substantial degree. Similarly, addition of CHO (carbohydrates) to a mixed diet does not increase hepatic DNL to quantitatively important levels, as long as CHO (carbohydrates) energy intake remains less than total energy expenditure (TEE). Instead, dietary CHO (carbohydrates) replaces fat in the whole-body fuel mixture, even in the post-absorptive state. Body fat is thereby accrued, but the pathway of DNL is not traversed; instead, a coordinated set of metabolic adaptations, including resistance of hepatic glucose production to suppression by insulin, occurs that allows CHO (carbohydrates) oxidation to increase and match CHO (carbohydrates) intake. Only when CHO (carbohydrates) energy intake exceeds TEE does DNL in liver or adipose tissue contribute significantly to the whole-body energy economy. It is concluded that DNL is not the pathway of first resort for added dietary CHO (carbohydrates), in humans. Under most dietary conditions, the two major macronutrient energy sources (CHO and fat) are therefore not interconvertible currencies; CHO (carbohydrates) and fat have independent, though interacting, economies and independent regulation. The metabolic mechanisms and physiologic implications of the functional block between CHO (carbohydrates) and fat in humans are discussed, but require further investigation. …”
[2] De novo lipogenesis in the liver in health and disease: more than just a shunting yard for glucose: “…Hepatic de novo lipogenesis (DNL) is the biochemical process of synthesising fatty acids from acetyl‐CoA subunits that are produced from a number of different pathways within the cell, most commonly carbohydrate catabolism. In addition to glucose which most commonly supplies carbon units for DNL, fructose is also a profoundly lipogenic substrate that can drive DNL, important when considering the increasing use of fructose in corn syrup as a sweetener. In the context of disease, DNL is thought to contribute to the pathogenesis of non‐alcoholic fatty liver disease, a common condition often associated with the metabolic syndrome and consequent insulin resistance. Whether DNL plays a significant role in the pathogenesis of insulin resistance is yet to be fully elucidated, but it may be that the prevalent products of this synthetic process induce some aspect of hepatic insulin resistance. …”