I suspect we’re only at the front end of realizing not all fat cells are the same at all.
‘ROS as a signalling molecule’ potential seems hugely important.
Because then it’s not looking at ‘if you have insulin it stuffs fat into into fat cells, unless your DNA says they can’t get larger’ or something…
…but instead, ‘insulin can be present all day if it wants, but every individual fat cell is only going to be open to it, or not, depending on its own individual setting…’
‘…and the setting is triggered to ‘closed’ by the ROS generated by saturated fat.’
Interesting: If a fat cell “does not respond to insulin” how did it ever get and keep fat in it to begin with?
My super-rough concept is that the body (the liver in charge of much of this) is constantly dumping out contents of fat cells into the river of blood, as minerals and more are in them and it’s a constant flow of resources being kept in realtime. And it’s just as constantly repackaging and restoring contents into fat cells. So a very living responsive but ‘realtime inventory’ system.
Basically… much like lipoprotein particles with cholesterol.
So maybe an adipose cell does not have a receptor related to insulin (god only knows why).
Still seems possible that the ROS-as-a-signalling-molecule may have some affect on the cell, though. Might be a different route we don’t yet know to look at or look for. I mean even finding that is relatively new research (especially in terms of this info bleeding through into the standard set of knowns or suspecteds in more than 3 people lol).
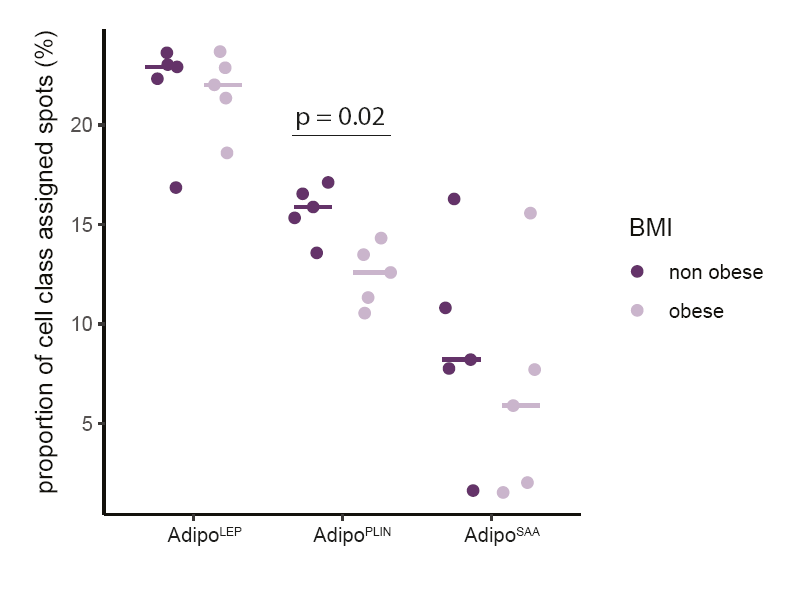
Maybe ‘the invite and/or pressure of insulin’ is not the only thing determining fat cell content, which is the big novel note in that chart in a way. That might reduce the scope or % of the proton theory even if it’s valid. I don’t think it would invalidate it. Might just indicate there is definitely more involved.
I wonder if a fat cell’s wall/container/membrane/whatever being insulin sensitive vs something else, is a little like how there’s cholesterol but then different kinds of lipid particles that ‘carry’ that and then different sizes and densities of each kind, and… maybe it will turn out a bit similar for fat cells, where the fat’s being carried around in the cell/as the cell, but what ‘type’ of cell detail is created to ferry it, depends on something else in the body.
Like in the body when ascorbic is low, venous tissue etc. wears and the body makes more small dense particles to use as bricks and mortar to shore it up. Remove the degradation, by correcting for the nutritional defiency*, and the DL %s change. How much of the shift in blood DL’s is due to reducing the chronic subclinical ascorbemia (*because the more animal foods and less carb foods esp. grains you intake, the less ascorbic you need)?
I am lipedemic, a syndrome without a known cure at the moment, since 1940 when it was officially named. I’m convinced this is trackable partly to a chronic subclinical deficiency in something I just don’t know what. Could also be too much of something toxic that ‘replaces’ something one needs and then is hard to boot out of place even if you add the needed content (heavy metals and halides do this in the body).
I once thought I’d figured it out, eons ago when I was reading (and praying and meditating and dreaming) on it regularly: weirdly enough pretty well everything about lipedema could be totally explained IF it were caused by low iodine. Or to put it another way, low iodine actually causes the same specific kinds of symptoms, fibrous tissue growth with edemic inflammation in it, it’s neither muscle nor fat so working on either of those does not affect it. In the case of low iodine it will specifically turn up in predictable areas though, it’s “dysplasia” in breast tissue as one example. Lipedema isn’t specific in that way but rather, simply affects fat cells, it appears, and I suspect the body then moves those cells to where they are least accessible to the vital organs (because the fat is mutant/damaged), and since nearly all lipedemics are women (or have that hormonal profile), it stores ‘hormonally’ – in the hips/thighs/calves for women, sometimes (usually later or when very large) in upper arms.
“Something is wrong with the fat cell” is mostly all that’s known right now it seems like. It’s one of those things likely underlying a HUGE % of the health problems in women in our culture (maybe men and we don’t realize it) so any real effort to truly figure it out, vs. have an eternal funding income related to it, I’ve become cynical about. Lack of understanding about the detail of adipose tissue is a lot of this though. Seems obvious to me the fat cells are the symptom not the cause. It ‘often but not always’ seems trackable to either families or locations, it is triggered by high hormonal events (puberty, pregnancy, megastress), and it gets worse as people get older (perhaps in part simply because it doesn’t get solved, so the problem is cumulative).
I would be curious to see, like in the research study with the graph you posted, if it was the same for men and women. Since there is so clearly a major diff in ‘some’ adipose in lipedema but that is so heavily geared toward women (one guesses estrogen related). I used to think lipedema was ‘twinkie fat’ – bad fats causing mutant fat cells that couldn’t be used for the liver’s body-wide warehousing really, lived nearly forever because it was like plastic, and was sometimes stiff, or leaky, or not permeable, resulting in a nightmare edemic ‘swamp’ of inflammation, edema, etc. in a cycle. I don’t know if I still think that’s the likely case anymore. It might be less something toxic than simply something deficient. (I got this partly from a sort of metaphysical ‘intuitive insight’ essay-experience one day. That all health issues that were not ‘acute’ injury or poison were actually deficiencies. Because the body was capable of handling anything else and compensating, but for that situation. It’s just that sufficient deficiency causes symptoms that eventually seem like they are one of the first two.)
As an example, eons ago research showed reducing calories extended life. So calories were bad. Then it showed that actually it was meat that was a problem. Meat was bad. But wait no it showed that only red meat was a problem. Steak was bad. But wait no it showed that the amino acid methionine was a problem. Methionine was bad. But wait no it turns out it was a deficiency in Glycine which is needed to deal with the methionine. (Because it seems every nutrient in our body has a sort of yin/yang – like calcium magnesium for example, or potassium sodium – might be similar for some aminos as well.) So in the end after so many years and so many THIS IS BAD conclusions it all turned out to mostly just be an issue with not getting enough glycine so it was an imbalance. I am just tempted to think there might be something like this going on with the adipose tissue.
Edited to add: a friend of mine with lipedema took a pretty major dose in 2-3 different routes of iodine for at least 18 months and it had zero effect on her lipedema. So… it ain’t that. Bummer because gosh I thought I’d stumbled on it.
The only thing that has worked for her is high dose ongoing serrapeptase. That improved my vision, totally healed my severely damaged from whooping cough lungs – no idea if it’ll help lipedema, it seemed to want to do those other things first neither of which I expected. But it’s more like a symptom treatment.
It eats dead protein, so dysplasia of any kind (it’s fantastic for when my fibroids grow and hurt, it can fix the pain within hours and reduce them within a couple days) basically gets dissolved by it. The more the tissue scaffolding is dissolved the less fat-edema is being held in it, so it has tangible results. Diff corps have diff coatings on the pills though so one has to find one that works for them, no point it taking it without a good enteric coating, and it’s frakkin expensive as a high-dose supplement. Miraculous for many people with scar tissue and more though.