This is a great point. I have been trying to reconcile Ted’s ideas with the whole “eat fat to satiety” thing lately and I still really can’t. Is it safe to say that if your fasting insulin somehow lowers but you continue to eat exactly the same, you would burn additional body fat?
Restrict plate fat when trying to lose body fat - discussion
dude there are so many nuggets of gold from @richard in this thread, I fucking love it. I love learning more and more about the science behind this stuff. So it seems the real question to ask for ppl who are stalled in weight/trying for the beach body or whatever, not how to cut your calories but how to lower your basal insulin long term. Seems like a much less straightforward proposition unfortunately.
Yeah I noticed that too. Remarkable isn’t it.
From a CI:CO worldview you could probably observe that Insulin resistance goes up and down with body weight and assume that body fat % drives IR up and down. Although as Gary Taubes points out the inverse is more likely, and a mechanistic explanation for that exists.
Insulin resistance is a survival adaptation to dealing with an energy glut. It makes sense that insulin sensitivity would be a survival response to an energy crisis. The problem of course is that their RMR drops and stays low.
Their exercise regime stayed high. Their RQ showed that they maintained a high protein low calorie diet … but I’ll wager they weren’t as hard core for 6 years. Seeing what happened to their insulin (and HOMA:IR) is a cautionary tale.
Weight regain is normal after weight loss from caloric reduction. I’ve seen studies showing that 97% of dieters regain everything and more after 3 years.
I’ve kept my weight gain off for 3 years on an ad libitium diet. That is magic right there.
Sure. But at some point I would expect your insulin would slowly rise a little to defend further weight loss … and then if you are eating to satiety you would naturally eat more.
One theory is that anything that does not stimulate insulin keeps you in a fasted state and BPC does not stimulate insulin.
What I don’t understand is why there is disagreement that CICO works for some people. No one is saying that CICO works for everyone, so why is the counter-argument that CICO works for no one?
As @richard and @CanKeto agreed upon: keto + eating to satiety can result in a “caloric deficit” which then leads to “weight loss”, so why all the pushback re: calories are garbage?
Even the anti-CICO quip “while you’re doing arithmetic, your body is doing calculus” still acknowledges there is math going on!
I accept and applaud that people have embraced the keto WOE and have lost weight without having to count calories. That is awesome!
Would it be more ketogenicforums.com friendly to refer to “food satiety units” instead of “calories”? There is so much baggage here. No, the human body is not literally identical to a bomb calorimeter, but can we not agree that the body is still subject to the laws of thermodynamics? Do we need to go all Jack Kruse-style and rewind all the way back to sunlight before we find common ground?
LOL Nup.
Just pointing out that in a time when food comes to you, being lean may be a viable fueling strategy.
When we had to chase it down, however - function strength and some long range tanks were more appropriate.
That is probably why as a species we conserved the mammalian hibernation reflex, AKA type 2 diabetes.
keto + eating to satiety can also lead to a “caloric surplus”. If for example, you were underweight because your gut under-absorbed carbohydrates and you then transitioned from a balanced diet (60% carbs) to a keto diet you will likely put weight on until your body reaches a stasis.
At that point keto + eating to satiety should lead to a gentle hysteresis which is an oscillation up and down around a stasis point.
That is really my point, that type 2 diabetes is a disordered state where we were over-absorbing energy, sometimes for many decades. In that scenario keto gives our bodies control over fueling, and our now ordered fueling systems puts us into a caloric deficit.
But we will also reach a stasis, and then a gentle seasonal hysteresis around that point.
We can always try to subvert that control by starving, or gorging but the 1st law of thermodynamics will require a re-balancing elsewhere - and not always where you think.
If you take in too little energy, yet have high insulin you probably won’t draw down much body fat, instead you’ll likely lose lean mass and your body will make cutbacks elsewhere. If you take in too much energy, but have extremely low insulin then you won’t be able to store much of that excess energy and will fritter it away in futile cycles (extra body heat, crazy legs, etc).
Calories in vs Calories out is inadequate to predict what a body will do, because it assumes that body fat is a passive reservoir that is always filled with excess and emptied by insufficiency.
The argument of the fungibility of calories (the ability to replace one for another without any change in stored energy) is not my problem with the Energy Balance hypothesis, nor is it really central to that hypothesis any more than the theory of gravity is dependent on a meter being a meter.
I really have 5 problems with the Energy balance theory;
- It oversimplifies energy consumption
- It assumes an impossible accuracy with energy intake
- The assumption that body fat always releases energy
- The math doesn’t check out
- The moral issue
1. The problem with energy Consumption
The theory lumps all energy expenditure OTHER than discretionary exercise and the energic cost of digestion into a black box called the resting metabolic rate (RMR). This is then treated as a value that doesn’t change and used along with exercise and how much protein is in your meal to determine your “Calories Out”.
The reality is that our RMR changes based on what we just ate, how much energy is in circulation, what hormones are acting upon adipose tissue, how much activity we are doing, how hydrated we are, the status of our essential nutrition.
Experimentally we’ve seen caloric restriction drop RMR by as much as 25% (biggest loser 6 year followup), and caloric over supply increase it by as much as 400% (Ethan Sims Vermont prison overfeeding study).
2. The problem with counting calories
“Calories In” is also subject to imprecision, but even still the fancy that we can count the number of calories being consumed flies in the face of the inbuilt inaccuracy of our labeling laws, unpredictable changes in gut absorption rates, the contribution from microbiota, and the calories that exit the gut un-absorbed.
Even the most rigorous calorie counters are off by up to 20%, for a person eating 2000 calories a day that is an inaccuracy of 1/9th lb a day, or ±42 lbs a year.
3. Assuming body fat is willing to release energy
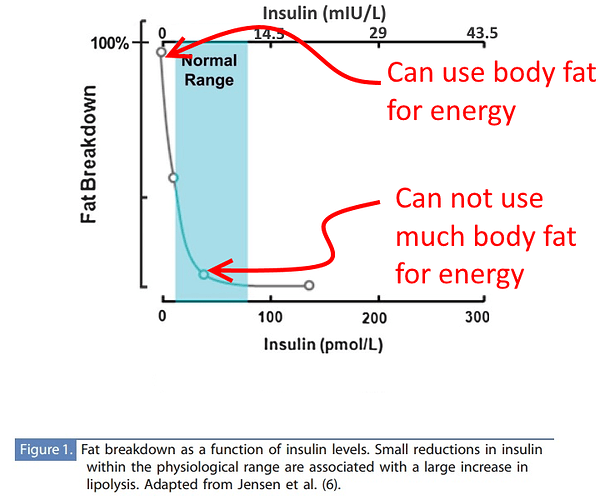
The amount of energy we can get from body fat will be constrained by how much insulin is in circulation, and the daily transaction limit for getting energy out of body fat.
If you are secreting more than about 13 mIU/l of insulin then you will have the same contribution of stored energy as someone who has almost no body fat at all. And even if you have virtually no circulating insulin, you will still be able to access only 31.5 kCal per day for each pound of body fat.
4. The problem with the math
The theory asserts that if you could accurately calculate Calories in, and Calories out then you could predict calories stored, but putting aside the impossibility of either of those as I’ve already discussed - the math doesn’t work because it’s not a simple function.
“Calories Out” changes based on “Calories In” so as soon as you think you’ve calculated caloric expenditure and turn your focus onto the caloric input - any change you make will change calories out again. The function is iterative, that is it changes every time you calculate it. Trying to use it to predict calories stored is like a dog chasing it’s tail.
5. The moral issue
But for me by far the biggest problem I have with CI:CO is that it moralizes a disease condition - it frames obesity a punishment for the sins of gluttony and sloth. It blames the victim.
That … and of course it doesn’t actually work to alter the disease state for the above reasons.
The reality is, in 99 cases out of 100, when you change the diet so obese people make less insulin by restricting sugar starch and protein - they rapidly lose weight and more importantly the biomarkers of the diseases that travel with obesity (Diabetes, CVD, Hypertension) disappear.
Did those people all of a sudden stop sinning? Or is there a simpler explanation?
Oh wait I have 6 problems with CI:CO …
It has been used by Coca Cola to sell sugar water to kids. Coke funded thousands of researchers as part of their “Energy Balance Consortium” initiative to do research “proving” the energy balance hypothesis.
Is this ALWAYS the case? Like this literally happens whatever your intake is? Or does it happen over time/in conjunction with other factors?
yeah really, is modifying your fat intake downward the same thing as counting calories? Even if you literally don’t count anything, just remove stuff from the diet?
The point is that calories aren’t a useful measuring stick, for (among others) the reasons @richard laid out.
It is not a question of being purist, or excluding other views. The reality is that many here (@richard included, if not foremost) are focused on helping people with T2DM, and those with insulin resistance and other forms of deranged metabolism with high insulin. For those folks, counting calories, or focusing on anything relating to caloric measurement, is an utterly pointless exercise.
If you (or others who bring this up) are blessed to be sufficiently insulin sensitive that you can reduce calories as a means of getting to a lower body fat or lose weight, congrats, you won the genetic lottery.
The reason that CICO is routinely dismissed on these forums is that for those with metabolic derangement and high insulin, it simply DOES NOT WORK. Period. And attempting to focus on calories, or reducing energy intake when insulin is too high to allow for getting energy from one’s own body fat is likely to lead to additional metabolic issues including a lowering of resting metabolic rate.
It’s OK to disagree with the recommendations that don’t work for you. That’s why most of us who post here regularly also acknowledge that n=1 is a thing, and that metabolically, we can all be special snowflakes. But for those with insulin issues, CICO is a disaster, and it’s that group that is most in need of the advice offered here.
Yes. And I explained to you why some alternate views tend to receive short shrift on the forums.
Whether you say “CICO” or “caloric deficit” doesn’t change the math.
A caloric deficit when you cannot access body fat is apt to provoke metabolic slowdown. How much and how quickly is open to debate. A caloric deficit when insulin is sufficiently low to allow access to body fat may result in the use of one’s own fuel. But that’s the point of the “to sateity” part. Keeping carbs and protein in check, while eating fat “to sateity” should lead to eating an amount that allows the body to use its own fuel at a sustainable rate.
Again, the question isn’t whether alternate views are OK. It’s who we are primarily attempting to help. The message that is repeated like a drumbeat is repeated because it has the best chance of helping the most people with insulin issues.
Your quote of @richard’s response is completely compatible with what I said. If you can access body fat (i.e. you’ve driven insulin sufficiently low to liberate FFAs and have them in circulation), then you don’t need to consume as many calories. That is not the same thing as “caloric deficit” driving the burning of fat. Caloric deficit, to the extent that it exists, is a product of lowered insulin providing access to body fat.
May I remind you of the first reply you posted on this thread?
That certainly sounds to me like you are asserting that calories drives fat loss.
You also wrote:
The first sentence is the point of disagreement. It is only true if insulin is low. If it’s not, then you can “driv[e] deficit” all day long and it won’t help.
Hence why you do not understand why you are facing disagreement.
I’ve already allowed that n=1 is a thing, and you may well be able to “cut” and get your BF% into the teens using caloric deficit. That’s why I pointed out that you may have won the genetic lottery. It’s not an insult, and it isn’t meant to belittle your view. It’s meant to point out that your arguments proceed, as you’ve just conceded, from the assumption of low insulin.
I would wager that the majority of people here aren’t fortunate enough to have low insulin going in. Some, like @richard, can be fully keto and still have high basal insulin.
Perhaps you could stop feeling attacked long enough to realize that your assumption of low insulin isn’t necessarily germane to others, and that’s why the pushback on your “alternate view”.
Your n=1 experience is as valid as anyone else’s, but that doesn’t make it applicable to others, particularly those who have issues with getting and keeping insulin low.
The problem is we have lumped all the uses of energy we have that aren’t running on a treadmill or the energy to digest our observed meal into a black box called RMR or BMR (resting or basal metabolic rate). And we have assumed for the sake of making calculations work out, that it remains pretty much static. And so there has not been a lot of science done on how far that can swing over how short a period of time.
As I have likely mentioned before we know that caloric restriction can drop metabolic rate in 13 weeks in the case of those biggest loser competitors. I don’t recall how long Ethan Sims tried and failed to raise the body fat mass of one prisoner over 11% through overfeeding … but his MBR went from under 2000 kCal/day to over 10,000 kCal/day. His study was 6 months long, but I don’t know how quickly that MBR rise was observed.
This appears to be a more dynamic system than most people realize as was shown by Dr Stephen Phinney in one of his lesser known studies.
http://www.metabolismjournal.com/article/0026-0495(88)90011-X/abstract
They locked 12 overweight patients in a Metabolic ward for 4-5 weeks, where every single calorie they ate and expended could be measured. The participants were fed 720 kCal/day with enough protein to maintain muscle mass (1.5g per kg of ideal body weight). The candidates were then split into 2 groups
- The control group were completely sedentary for the entire time
- The intervention group performed 27 hours of supervised Cardio
- Common sense would tell you that the intervention group burned more Calories and ate the same amount so they should have lost more weight. Right?
Controversially, both groups lost a similar amount of weight in 4 weeks, 6.5kg for the exercisers, 6.9kg for the couch potatoes.
So the question you have to ask is
#“How did they lose more weight if they did less exercise?”
Well the researchers measured the actual energy use of the participants every moment of the time they were in the ward, both when they were on the treadmill and when they were at rest. For the first week the resting energy expenditure (REE) of both groups dropped by 10% – meaning the amount of energy their bodies used when they were just lying on a bed trying to not do anything dropped by 10% in response to the common Calorie restriction. After the first week the REE in the control group (Couch potatoes) stayed at that new level for the remainder of the experiment.
Where it gets very interesting is that the REE of the Intervention group (Exercisers) continued to drop by a further 17%. So what apparently happens is that when you restrict your food calories (diet) and do Cardio for as much as 2 hrs a day, it need have no net effect on your weight loss because your own bodies homeostatic energy regulation mechanism can conspire to make you lose fewer Calories in the 22 hrs a day that you aren’t running on the treadmill.
So that effect happens in days not weeks.
What we need is fundamental research to work out how much this re-balancing changes over hours. But it appears from Dr Phinney’s study that it changes in days. And from Ethan Sims and Kevin Hall we can see that it can range from -25% to +400%.
I think that is worth knowing more about.
If you insist on being patronizing you won’t get very far on these forums.
The problem isn’t the label.
The problem is the assumption that everyone SHOULD “drive” a deficit, and that a “deficit” MUST be acquitted from storage.
I don’t know about you, but I am tired of hearing me bang on about insulin inhibition of lipolysis … so I’ll just leave this chart here
According to population research in California and clinical research from Dr Joeseph Kraft the number of Americans that are hyperinsulinaemic is 52-85%. On this forum you might find that number is even higher, as out audience feeds from listeners to a podcast about metabolic disease. People hormonally inhibited from having access to adequate body fat for energy are in the significant majority.
“Would y’all feel better if we just called “Caloric restriction” something else?”
- No! Next question.
In this case, @Adam stated up front that he is still healing T2D and has plenty of extra fat. Perhaps your experience with metabolically healthy individuals would be better received in a different context.
But generally speaking, insulin resistance is present in a large number of overweight non-diabetics (and in some normal weight people) long before they lose glucose control. The T2D diagnosis means they have had high insulin for years without knowing it, because doctors do not routinely check it.