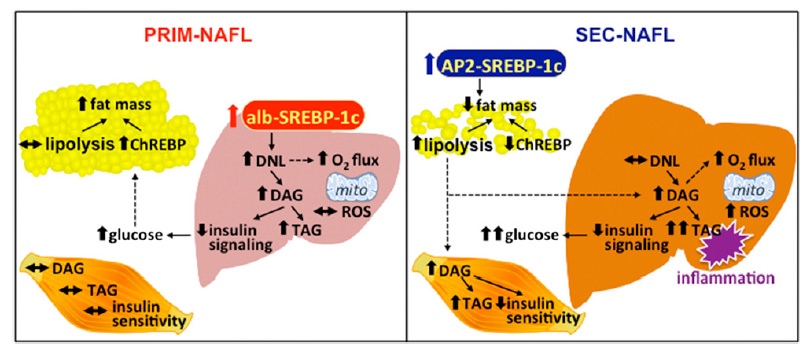
This study describes the differences between two pathways that can lead to NAFDL. The one called Primary (PRIM) begins with increased de novo lipogenesis (DNL) in the liver. The Secondary pathway (SEC) is a result of an increased free fatty acid FFA load on the liver coming from impaired adipose tissue storage.
First, these two routes have a common denominator; they both involve an adequacy of choline supply to export fats from the liver. That’s the part at the top involving alternate forms of SREBP-1c. SREBPs regulate the synthesis of phosphatidylcholine at several levels. Triglycerides created in the liver must be exported as VLDL. Masterjohn has written extensively about choline deficiency and fatty liver here:
https://chrismasterjohnphd.com/blog/2016/04/24/start-here-for-fatty-liver-disease/
There are also some genetic indicators of impaired choline sysnthesis here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1574369/
Now to the study at hand.
The PRIM pathway involves hepatic DNL. Creating fattty acids from fructose or alcohol substrates falls into this category.
Liver-specific overexpression of SREBP-1c and increased hepatic DNL in the PRIM mouse model leads to accumulation of DAGs and triacylglycerols (TAG) and development of NAFLD. NAFLD in PRIM associates with decreased insulin signaling and higher hepatic glucose output.
…ChREBP-mediated lipogenesis in adipose tissue and fat mass are increased, which could protect from hyperglycemia and peripheral IR.
Note this last part. Increased storage of fat in adipose tissue is protective against fatty liver accumulation in this model.
The SEC pathway does not involve an increase liver DNL, and is a function of adipose health. Overloaded adipose tissue releases FFA when insulin signaling can no longer keep fat in the fat cells. This occurs when a person’s adipose capacity is exceeded, regardless of weight. Healthy fat cells = properly stored fat and systemic insulin sensitivity. Unhealthy fat cells = runaway lipolysis and excess FFA delivered to the liver.
On the other hand, SEC mice are characterized by loss of adipose tissue and ectopic lipid accumulation in both liver and skeletal muscle… Liver and skeletal muscle are both characterized by decreased insulin sensitivity.
Moreover, accumulation of extrahepatic lipids in SEC but not intrahepatic lipids in PRIM associates with portal and lobular inflammation of the liver.
So, does fructose cause fatty liver? It depends.
In the PRIM model it would take an approprite level of fructose to overcome a lack of available choline, thereby trapping fat in the liver instead of exporting it to adipose tissue. BUT fructose also increases the insulin response to glucose and this will exacerbate the SEC pathway to fatty liver, in which liver disease is downstream of the effects of glucose and insulin.
The next post on this topic will involve inflammation and immune system responses and the role they play in insulin resistance… someday

 )
) , I feel better when I see this! Haha…
, I feel better when I see this! Haha…