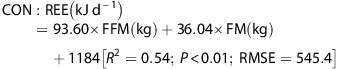
The problem with the CICO model that Dr. Fung made abundantly clear is that it’s a one compartment model. It fails to appreciate that the bodies compensatory mechanisms adapt to calorie restriction by lowering metabolic rate, adjusting hormones, etc in order to confound weight loss and cause weight regain. Even Dr. Fung never said CICO was completely wrong, just that it was inadequate, and doomed to failure because of the compensatory mechanisms of adaptive thermogenisis (decreasing RMR).
The following study is called the Matador study (Minimising Adaptive Thermogenesis And Deactivating Obesity Rebound). This study concedes the inadequacy of standard CICO protocol of continual calorie restriction, and focuses on minimizing the compensatory mechanisms the body uses to fight back against weight loss, chief among them adaptive thermogenisis (declining RMR). The hypothesis of the study is that if calorie restriction is done for two weeks, and then calories are brought back to maintenance for two weeks, the body’s adaptive mechanisms will essentially be short circuited, and weight regain will be minimized. That the metabolism can recover to steady state in roughly 2 weeks of refeeding has been shown in prior studies.
The study lasted for 32 weeks with alternating 2 weeks periods of calorie restriction and maintenance calories. Yes, there was a robust control group. Yes, the study was sufficiently powered. Yes, there was a 6 month follow up. Yes, results are absolutely stunning. Seriously, read the study. It’s very encouraging both in the sense that academia is beginning to concede that continuous calorie restriction is asinine, and because of the novel, intuitive approach used (2 weeks on 2 weeks off).
@atomicspacebunny, @OldDoug: This one is right up your alley.
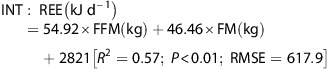
Adjusted RMR at 6 month Follow up
Continuous: -770 +/-523
Intermittent: -255 +/-515
Fat Loss During Study
Continuous: -8.0 +/-4.4
Intermittent: -12.3 +/-4.8
Fat Loss at 6 Month Follow Up
Continuous: -3.0 +/-4.4
Intermittent: -11.1+/-7.4


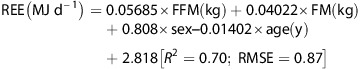







 Quite absurd! So, I suppose that a basic protocol or helpful remedy when exciting studies are conducted and published but are male-centered, involves acknowledging the issue straight on, so as to advance structured change on behalf of actual public health and expedient generational health.
Quite absurd! So, I suppose that a basic protocol or helpful remedy when exciting studies are conducted and published but are male-centered, involves acknowledging the issue straight on, so as to advance structured change on behalf of actual public health and expedient generational health.