Yes, those would be great! But actually they still wouldn’t answer the “is an ongoing high glucose level healthy?” question, especially since A1C is somewhat dependent on how long our hemoglobin lives (it’s generally three months, but could be longer or shorter, which would change the significance of that number).
Does a healthy ketogenic diet cause irreversible insulin resistance?
But if it’s not very glycated (i.e., HbA1C is low), then it’s much less susceptible to oxidative damage, as I understand it, and that has to be a good thing, all by itself.
@PaulL A1c is essentially a measure of how much glycation has happened over the life span of the hemoglobin, right? So when the lifespan is shorter, I think the 5.0 doesn’t mean the same thing (or, basically, it’s showing an artificially low number). And in Zimon’s case, it seems like his average would be higher based on the glucose readings he’s getting.
Just some guy? What does it matter?
Information should be evaluated based on the content of the information, not on the authorship. It is a logical fallacy, an argumentum ad verecundiam, to assert that something is true because it is presented by an authoritative source or that something is false because it is not.
If multiple doctors are expressing different, contradictory, opinions, then it is obvious that at least some of them are wrong despite being doctors. Even if all the “experts” are presenting the same opinion, it might well be that all of them have it wrong. What if “just some guy” states a view that is contradicted by “just some doctor” and you dismiss his view based on credentials while there may, at the same time, be many other academics that are in complete agreement with “just some guy” of whom you are ignorant?
Dr. Ansel Keys was, well he was more than “just some doctor.”
I grew up in a family of scientist, professors, so I know that they far from perfect, often pompous, prideful, human, often wrong, sometimes dishonest, and at times wonderfully objective and intellectually honest. I would never dismiss the views of “just some guy” based on a lack of credentials, it is not in my nature, rather I ask if what is asserted is rational and supported by data, just like any objective scientist.
The diet of many hundreds of millions of people, likely billions, has been impacted negatively by the views of Dr. Ansel Keys, an establishment view, while any rational “just some guy” could easily observe that there are peoples around the world, the Inuit, the Massai and others, peoples completely devoid of all of the diseases of western civilization, who have been eating LCHF for a great many generations.
I find more veracity in the observation that “just some peoples” have been eating LCHF disease free for a great many generation then the views of “just some doctor”. That is I trust my own ability to reason, to think rationally, more then the views of “experts”, who, when they get it wrong, lead enormous numbers of lemmings over the cliff
I think it important that everyone at least attempt to think for themselves.
Eat like an Eskimo.
Keto for Life!
Respectfully,
Richard
[on edit] I apologize for the rant.
tl;dr version: Per my doctor: No, the ketogenic diet does not cause irreversible insulin resistance.
Update:
Went to the doctor and asked if the ketogenic diet could or would change anything in me permanently and she said no. She also did not balk at my stating that I had read that the diet induces peripheral insulin resistance but rather nodded. She also said I may cheat from time to time, how ever often or little I like and that staying in ketosis will not cause diabetes or any other problems and that if I go back to a normal diet my body will adapt and go back to normal.
She also said that the ketogenic diet is not known to cause arterial stiffening and agreed that it should improve cardiovascular health (this is related to another thread of mine which I will also update).
Great thread here folks! I’ve been low carb for about 2 years, am now a healthy weight and just started seeing my morning BG increasing. My fasting insulin is 3 and my HbA1c showed my BG is 108, meaning my HOMA-IC score is .8 which is in the Optimal category. I recently found two links that may help folks. One is a great article from Diet Doctor on this https://www.dietdoctor.com/low-carb/fasting-blood-glucose-higher and the other is a HOMA-IC calculator that gives you optimal ranges. https://www.thebloodcode.com/homa-ir-calculator/ That said, I’m now considering some sort of carb cycling as an experiment to test this theory.
I started adding a few carbs to my diet to see how I did. I started with a extra carbs every 3 days which led to my having a confidence that I could switch from sugar to fat easily any day. I would have maybe as much as 80 carbs in a day. Soon I started feeling like crap with night sweats and poor sleep. I’ve come to the conclusion that I was actually having nocturnal hypoglycemia. I did a 2-day fat fast and no more night sweats or trouble sleeping. I think it’s time to invest in one of those smart devices that tracks BG all day. I wish I had a doctor I could share this info with. I know I would get a lecture if I talked to my current MD.
What was you BG or insulin before you started keto?
Also, if you are in the US you will need a prescription for a continuous blood glucose monitor like the Freestyle Libre
I never checked my bg before except for yearly blood work with my doc. It was always around 110. It’s still at least that high in the morning and I started keto in Oct 2017. About 3 months in I had a fasting insulin of 10. I’m 56 now so I’m wondering how much can I actually repair my metabolism at this point. I work from home but my job is stressful so that throws dirt on my trail as well.
Fry, I enjoyed reading all your responses. Any new updates? I am replying just to keep this awesome discission going. I am still not understanding why it’s ok to have higher fasting BG while on keto … high BG is high BG, regardless of the reason and we know high BG is not good. Saying your BG is high because your insulin is low on keto makes it sound like T1D (just for analogy purpose, I know T1D is a million times worse).
Awesome discussion. Any new updates or a new thread with latest discussion? I am replying just to keep this awesome discission going. I am still not understanding why it’s ok to have higher fasting BG while on keto … high BG is high BG, regardless of the reason and we know high BG is not good. Saying your BG is high because your insulin is low on keto makes it sound like T1D (just for analogy purpose, I know T1D is a million times worse). If anyone has found any new studies that answers this iam interested. Thanks!
It’s all relative, but the simple explanation has to do with glucose sparing by the muscles, once they are fat-adapted. Serum glucose is tightly regulated, if we are not jacking up the level with an excessive carb intake. It naturally rises and falls throughout the day, but should stay within a fairly narrow range. Dr. Paul Mason, the Australian sports physician, says that he’d rather see stable levels in his patients, even if they are what some would consider high, than wild fluctuations.
As for “adaptative glucose sparing,” also called “physiological insulin resistance,” here is an explanation:
Fascinating. Not sure I fully grasp every nuance, but the different needs of muscle vs brain tissue for glucose provides an “a-ha” moment for me.
My understanding is that the brain given ketones as an option will select the ketones for fuel even when it has glucose as an option. In other words, when available, ketones are the preferred energy option. When you see the differences between ketone and glucose metabolism you understand why this is probably so. Ketones yield more energy per unit and produce less waste to deal with. I may have got this from one or several of Bikman’s talks, but can’t cite anything at the moment.
I interpret the brain’s ketone preference to mean that given sufficient time to adapt and sufficient ketones, the brain’s demand/need for glucose will gradually decline. There’s some debate about just how much of the brain’s energy requirement can be met by ketones - some think it maxes out at about 2/3 to 3/4; this is the current paradigm. Bikman thinks ketones could satisfy 100% with full adaptation and sufficient ketone availability. Whatever the ultimate total of energy supplied by ketones, as the brain uses more ketones for energy gluconeogenesis should scale down, since the brain has the biggest demand for glucose and if it’s demand decreases then the synthesis of glucose should follow.
I note that in the article cited by @PaulL , Peter says “I spend rather a lot of my life in mild ketosis” and I suspect that the fasting blood glucose rise noticed by Peter and others might in fact be due to having insufficient ketones available for the brain to max out, so it’s demand for glucose remains. As long as the brain says “feed me!” gluconeogenesis is there to do just that. When the brain stops asking for more glucose, I think gluconeogenesis stops making so much.
This would help explain why exogenous ketones have been observed to lessen the symptoms of brain disfunction among older folks who are still eating SAD. If indeed the brain prefers ketones it’s not going to be particularly fussy about whether you ate them or synthesized them in the liver. All that matters is they’re available and it uses as much as it can.
I have to go to work, so I don’t have time at the moment to comment. But I also think this might have significant bearing on another ‘mystery’ for those of us who have been keto for several years and experience a marked reduction in measurable ketones. More later!
PS (Next day!) Finally getting time to follow up. See following posts.
Comments in following post. I will there draw attention to items in the diagram and quote portions of the paper. I’m posting the diagram and the paper here separately for easier reference.
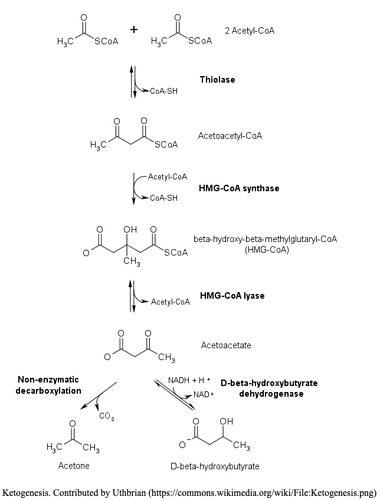
Here’s the flow diagram of ketogenesis copied from here. They in turn copied it from here. They don’t cite where they got it. But it’s a common diagram so they could have got from virtually anywhere. This is the standard diagram.
Here are the papers:
Same here, the whole adaptive glucose sparing thing always confused me, but I did notice after years of strict keto that when I did eat carbs my body completely over reacted to it, whether that’s more like a resistance or not I don’t know, but feeling like crap and then fighting consciousness isn’t fun. I do TKD now and that doesn’t happen anymore. Seems to simultaneously make sense… and not.
My question is ‘what might limit ketogenesis in long-term fat adapted individuals?’ A secondary related question is it something to be concerned about? Do we just go with the flow and accept it as a natural outcome? KCKO, etc.
The experience of greatly reduced ketones after being on keto for several years and presumably fat adapted has been noted by multiple posters here on the forum.
This is going to be a long post. So I shall break it up into pieces. This is the first piece.
Let’s first get the initial parameters out of the way. I’m talking about folks who are in long-term ketosis. These people have eaten a standard keto diet defined as ‘high fat’, ‘moderate protein’ and ‘very low/no carbs’. Pretty much Phinney and Volek’s definition of the nutrional keto diet. I’m also talking about folks who have remained consistently in nutritional ketosis for several consecutive years. By ‘consistently’ I mean specifically keeping carb intake and resultant glucose/insulin levels sufficiently low as not to interfere with continuous ketosis. This excludes anyone doing alternative keto diets such as: TKD, CKD and HPKD. Or any other iterations that intentionally/accidentally interrupt continuous ketosis whether on a regular basis or not. It’s your business not mine if you’re doing any of that, but I don’t think your experiences are relevant to answering my questions.
From Biochemistry, Ketogenesis
Mechanism
Ketogenesis occurs primarily in the mitochondria of liver cells. Fatty acids are brought into the mitochondria via carnitine palmitoyltransferase (CPT-1) and then broken down into acetyl CoA via beta-oxidation. Two acetyl-CoA molecules are converted into acetoacetyl-CoA via the enzyme thiolase; this is also known as acetyl coenzyme A acetyltransferase (ACAT). Afterward, acetoacetyl-CoA is converted to HMG-CoA via the enzyme HMG-CoA synthase. HMG-CoA lyase then converts HMG-CoA to acetoacetate. Acetoacetate can be converted to either acetone through non-enzymatic decarboxylation or to beta-hydroxybutyrate via beta-hydroxybutyrate dehydrogenase.
Acetoacetate and beta-hydroxybutyrate are the two ketone bodies used by the body for energy. Once they reach extrahepatic tissues, beta-hydroxybutyrate is converted to acetoacetate via the enzyme beta-hydroxybutyrate dehydrogenase, and acetoacetate is converted back to acetyl-CoA via the enzyme beta-ketoacyl-CoA transferase. Acetyl-CoA goes through the citric acid cycle, and after oxidative phosphorylation, produces 22 ATP per molecule. Acetone does not convert back to acetyl-CoA, so it is either excreted through urine or exhaled.
Right away, I can see multiple points of potential issues. Fatty acids are delivered to the mitochondria for processing via Carnitine Palmitoyltransferase (CPT-1). What happens if CPT-1 is not functioning normally or not produced in sufficient quantity? What if CPT-1 is ‘decoupled’ and turning fat into lost heat, as described by Bikman in his talks about BAT? What if Bikman is substantially correct that being in ketosis gives one a ‘metabolic advantage’ and that advantage is the decoupling of CPT-1 such that you’re blowing off more energy in the form of wasted heat rather than ketone synthesis? That could explain the whole thing in a single sentence. Maybe.
According to Biochemistry, Ketogenesis, after being brought into the mitochondria via CPT-1 fatty acids are then 'broken down into acetyl CoA via beta-oxidation. But that may be an outmoded description because according to The Definitive Guide:
Acetyl-CoA Formation through Fatty Acids
Acetyl-CoA formation is also said to occur via fatty acid catabolism; however, it is now understood that this acetyl-CoA is a product of carbohydrate metabolism. As acetyl-CoA can be converted into lipids and vice versa it is sometimes confused with a separate role; its true role is as a monosaccharide (glucose) metabolism catalyst.
This agrees with a comment I read from @amber in one of her blog posts about why we might have low ketones years into ketosis - the limits of acetyl-CoA due to our reduced carb consumption. Sorry I can’t cite the post, but I’ve noted it in another post, so may be able to find it and add it here.
So if we can expect lower acetyl-CoA as a result of low/no carb intake, how exactly does that impact the very first step of the process? Is some fat converted to acetyl-CoA? If so, how much? Does that amount vary individually? Or is no fat converted and gluconeogenesis has to make some glucose so it can catabolize into acetyl-CoA so the fat can catabolize further? Do we, in fact, have to synthesize some amount of glucose in order to synthesize some amount of acetyl-CoA to burn fat?
We’re not even down to:
- Two acetyl-CoA molecules are converted into acetoacetyl-CoA via the enzyme thiolase. What if you have a thiolase deficiency?
- Acetoacetyl-CoA is converted to HMG-CoA via the enzyme HMG-CoA synthase. What if you have a HMG-CoA synthase deficiency?
- HMG-CoA lyase then converts HMG-CoA to acetoacetate. What if…
I can see this is going down a rabbit hole real fast. More to come. 
Long term Keto and ketones
Thanks for the mention. The post you want is this one: Keto-adapted but no (low) ketones? Part II
I have just a couple of comments. First, the uncoupling idea wouldn’t have to do with CPT1A. CPT1A escorts the fat into the mitochondria. If you have a problem with that, you would end up with issues with both ketogenesis and gluconeogenesis. I described this case in the paper about the Arctic variant, which is linked to at the top of the post above. Slow CPT1A can be overcome with factors like high PUFA intake.
If it’s uncoupling, which happens in the mitochondria, this happens after fat is metabolised but before ATP is made with the proton gradient. I’m pretty sure ketogenesis would still happen here. In general, the more uncoupling, the higher the ketosis.
The enzyme deficiencies you mentioned, if you had them would mean you would never have high ketones. That is, this should be evident already before keto-adaptation, unless you’re suggesting that the deficiencies happen as a result of keto-adaptation?
As I mentioned in the article, I think the most likely explanation is simply lower fat to protein ratios in many lean keto-adapted people.
Long term Keto and ketones
Thank you for clarifying several points!
Yes, in fact I wondered if keto adaptation might cause reduction in some enzymes. Something has to change over time. My initial presumption was the diet remains essentially constant - resulting in consistent and continuous ketosis. Of course, if one is not consistently in ketosis all bets are off.
I’m currently testing your fat:protein ratio idea. For about 9 months I increased my protein intake to 150 grams and reduced fat intake to 222 grams per day. Aug 01, I changed back to my former ratio of 120 grams of protein and 240 grams of fat. Total calories remained approx the same: 2650-2700 daily. Although I generally eat within a 2400-2700 ‘caloric window’.
When I first got my Ketonix in 2019 I was eating to my prior ratios of 2:1 fat:protein grams. I was averaging 20-50 ppm acetone consistently daily, throughout the day. For whatever it’s worth - at the very least it confirmed consistent ketosis. I’m not convinced that acetone indicates much of anything other than you’re breaking down acetoacetate so must have some measurable level of ketones. I am currently blowing sub-10 ppm and usually sub-5 ppm multiple times per day. So I’m generating much less acetone. For whatever it’s worth - at the very least it confirms consistent ketosis. Just a lot less! I have to admit that I have not measured ketones for a year and a half, so I don’t really know exactly when the drop started and whether or not it corresponded to changing my fat:protein ratio about 9 months ago. I also don’t donate blood, so I have no idea of what my β-hydroxybutyrate levels are or how they vary during the day. I must have some because I’m in ketosis and still conscious.
So far my acetone still tests sub-10 ppm as before changing back my macro ratio. I am also eating a ‘coconut casein’ pudding every morning to up my exogenous MCT intake. My ‘pudding’ consists of 33.4 grams of casein and 25 grams each of coconut oil and MCT oil.
Thanks again for responding.
Long term Keto and ketones