I have just ordered a few books…
“Nature Wants Us To Be Fat” by Richard Johnson
“Drop Acid” by Dr. David Perlmutter.
Has anyone read either of these and formed an opinion on the theory, which I believe came from Richard Johnson’s research?
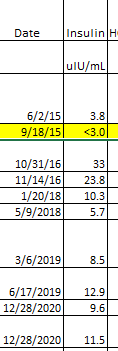
My interest is due to my extreme insulin resistance and high uric acid and homocysteine levels and low folate.
I have recently adopted a carnivore diet, due to high inflammation caused by rheumatoid arthritis and IBD.
I also have very low iron levels (due to IBD and poor absorption of nutrients).
Have been eating a lot of liver to try to get iron levels up but resorted to an iron infusion this week, when I realised that purines in organ meats raise uric acid levels and if Johnson is correct that is why my insulin has skyrocketed.
Another catch 22. Seems like the more I learn the less I can eat!
Taking Quercetain to drop the uric acid and folinic acid to get my Folate up and homocysteine down.
And recently started on compounded Low Dose Naltrexone, 2 mg a day, to address the IBD (hopefully).