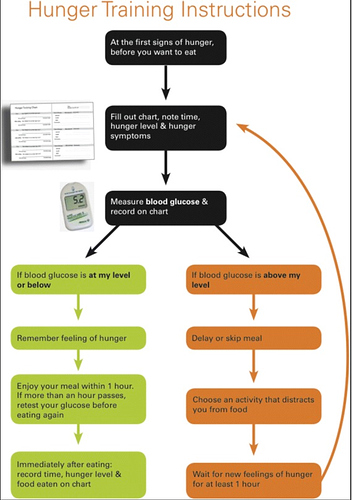
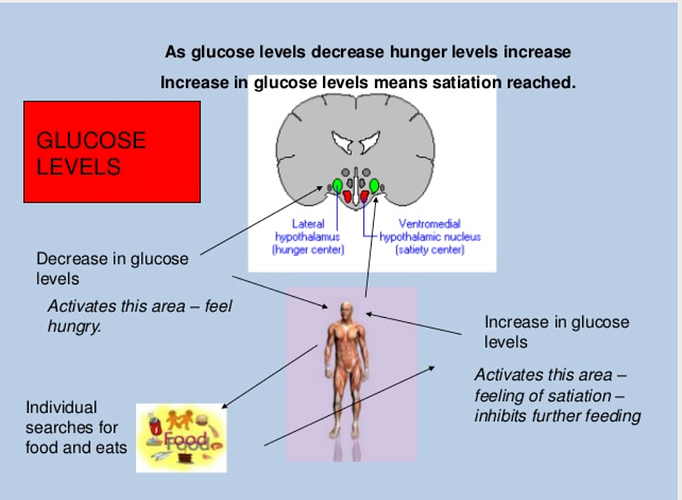
That is why I would eat when I’m hungry but not sugar (sweets). I like to pay careful attention to that hunger “craving” signal because that is the survival mechanism and reward signal of the brain and body, that is the signal I use to train (from my high carb\sugar addiction) my body to space out my meal windows using a glucose meter. It works like a miracle for me when combined with the ketogenic diet and intermittent fasting ratios (adapting the metabolic homeostasis to one meal a day OMAD and not hungry).
Blood glucose levels still matter even on a ketogenic diet because glucose is the master regulator of the leptin, ghrelin, insulin, glucagon, IGF-1 and the level of its presence creates the homeostasis of the entire metabolic regulation of the body because we are made of sugar and that does not mean we stuff our body with excessive amounts of it.
Of course you will see a lot of research on the subject that come up with some quirky paradoxal conclusions, that try to paraphrase a conclusion “…that’s not it” or “…it’s more complex than we thought” …it cannot be anymore complex than the quality of food we lift to our mouth and how much of it we eat.
References:
- “… Blood glucose has long been considered a biomarker of hunger [1]. …This condition of hunger was associated with glucose concentrations of 80 mg/dL or lower in humans [1,3-6] and was exacerbated by injection or infusion of insulin [7]. Blood glucose has a central role in the regulation of energy metabolism. …” “… Background: The will to eat is a decision associated with conditioned responses and with unconditioned body sensations that reflect changes in metabolic biomarkers. Here, we investigate whether this decision can be delayed until blood glucose is allowed to fall to low levels, when presumably feeding behavior is mostly unconditioned. Following such an eating pattern might avoid some of the metabolic risk factors that are associated with high glycemia. …More
- **Appetite regulation by carbohydrate: role of blood glucose and gastrointestinal hormones. ** “…This study has shown that the effects of intestinal glucose on appetite are not mediated via an increase in blood glucose but are likely to reflect small intestinal stimulation of release of either insulin or intestinal incretins. …” …More
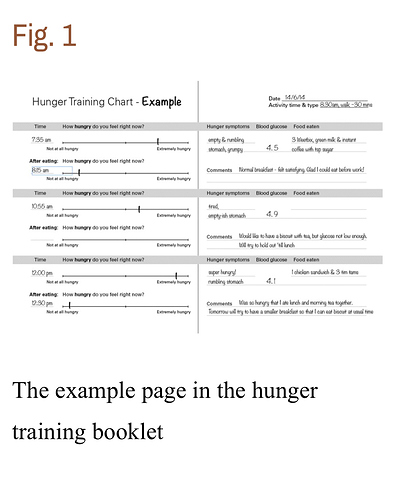
- Adherence to hunger training using blood glucose monitoring: a feasibility study
Background: “Hunger training”, which aims to teach people to eat only when blood glucose is below a set target, appears promising as a weight loss strategy. As the ability of participants to adhere to the rigorous protocol has been insufficiently described, we sought to determine the feasibility of hunger training, in terms of retention in the study, adherence to measuring blood glucose, and eating only when blood glucose concentrations are below a set level of 4.7 mmol/L.
Method: We undertook a two-week feasibility study, utilising an adaptive design approach where the specific blood glucose cut-off was the adaptive feature. A blood glucose cut-off of 4.7 mmol/L (protocol A) was used for the first 20 participants. A priori we decided that if interim analysis revealed that this cut-off did not meet our feasibility criteria, the remaining ten participants would use an individualised cut-off based on their fasting glucose concentrations (protocol B).
Results: Retention of the participants in the study was 97 % (28/29 participants), achieving our criterion of 85 %. Participants measured their blood glucose before 94 % (95 % CI 91, 98) of eating occasions (criterion 80 %). However, participants following protocol A, which used a standard blood glucose cut-off of 4.7 mmol/L, were only able to adhere to eating when blood glucose was below the prescribed level 66 % of the time, below our within-person criterion of 75 %. By contrast, those participants following protocol B (individualised cut-off) adhered to the eating protocol 84 % of the time, a significant ( p = 0.010) improvement over protocol A.
Conclusion: Hunger training appears to be a feasible method, at least in the short-term, when an individualised fasting blood glucose is used to indicate that a meal can begin. .…More