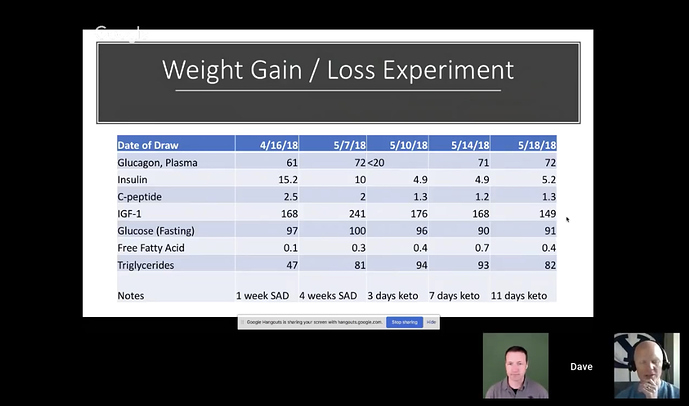
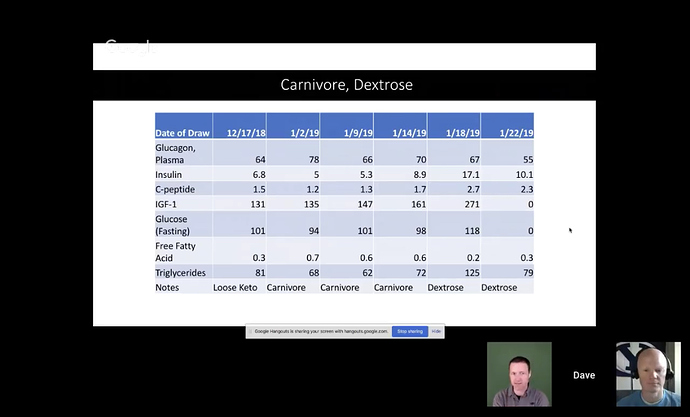
I disagree, especially for those of us lww carb/keto for 5+ years. When I started out, I could get blood ketones over 3.0, no problem, even eating. Now, most days I start under 0.5 and it goes up all day, but rarely above 1.0, and even 36 hour fasts don’t get it to that level… I just did a 4.5 day fast, and the highest measured value I got was 1.9. And then I transitioned into 3 days of high fat, high calorie (Dave Feldman’s protocol), and my ketones went down. Down. And I’ve been guzzling cream, sour cream, and other high-fat foods.
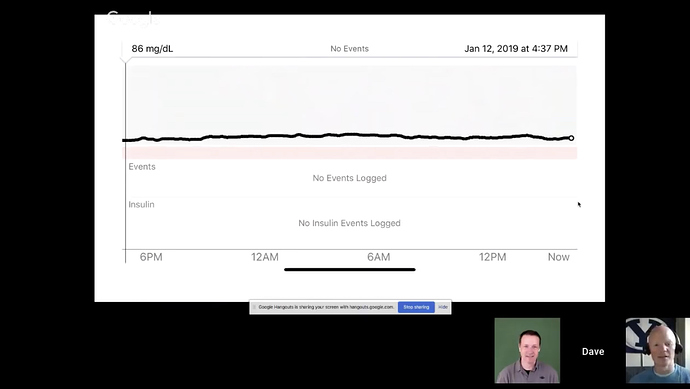
At some point, you become very efficient with ketones. And my blood sugar is always “high” in the mornings if I’m eating. (Went from 72 4.5 days into the fast to 108 this morning, two days after stopping the fast, while eating a TON of fat.) Yet, I’m down about 60 pounds and have gained about 10 pounds of muscle (will know more at my next DEXA scan).
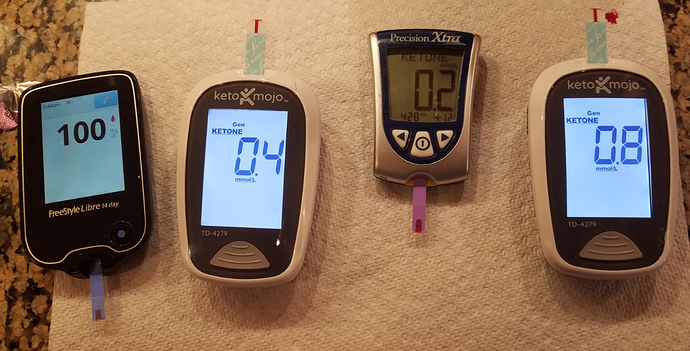
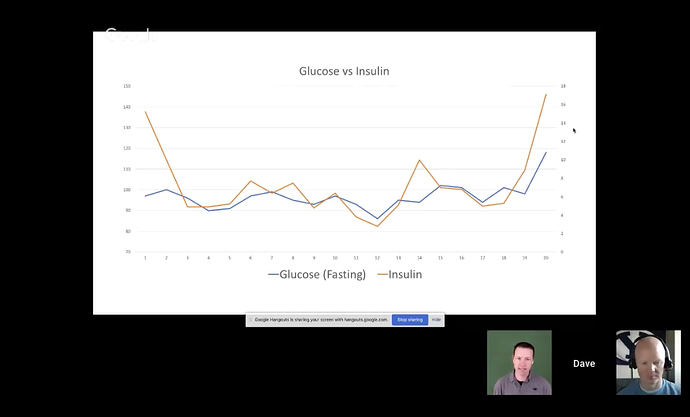
After testing almost 1,900 times with blood sugar (4 different meters), ketones (two different blood meters, ketonix for breath, and urine stirips), I’ve given up on testing. Furthermore, my insulin has been all over the map:

My fasting insulin is all over the map, while my HbA1c keeps going down and I keep losing weight. That doesn’t quite compute. (The ones highlighted in yellow were after 4.5 days of fasting.) I started low carb 1/1/14. The test on 3/6/19 was in the afternoon, fasting, but I had coffee and tea (both no cream) earlier in the morning. The other tests in the morning.




 Ok so I have a lot more reading now and reviewing. Who is Richard?
Ok so I have a lot more reading now and reviewing. Who is Richard?